EHR Software Development: How to Build a System in 2025?
Overflowing file cabinets and misplaced patient charts are fading into the past. How come? EHR software development is the answer.
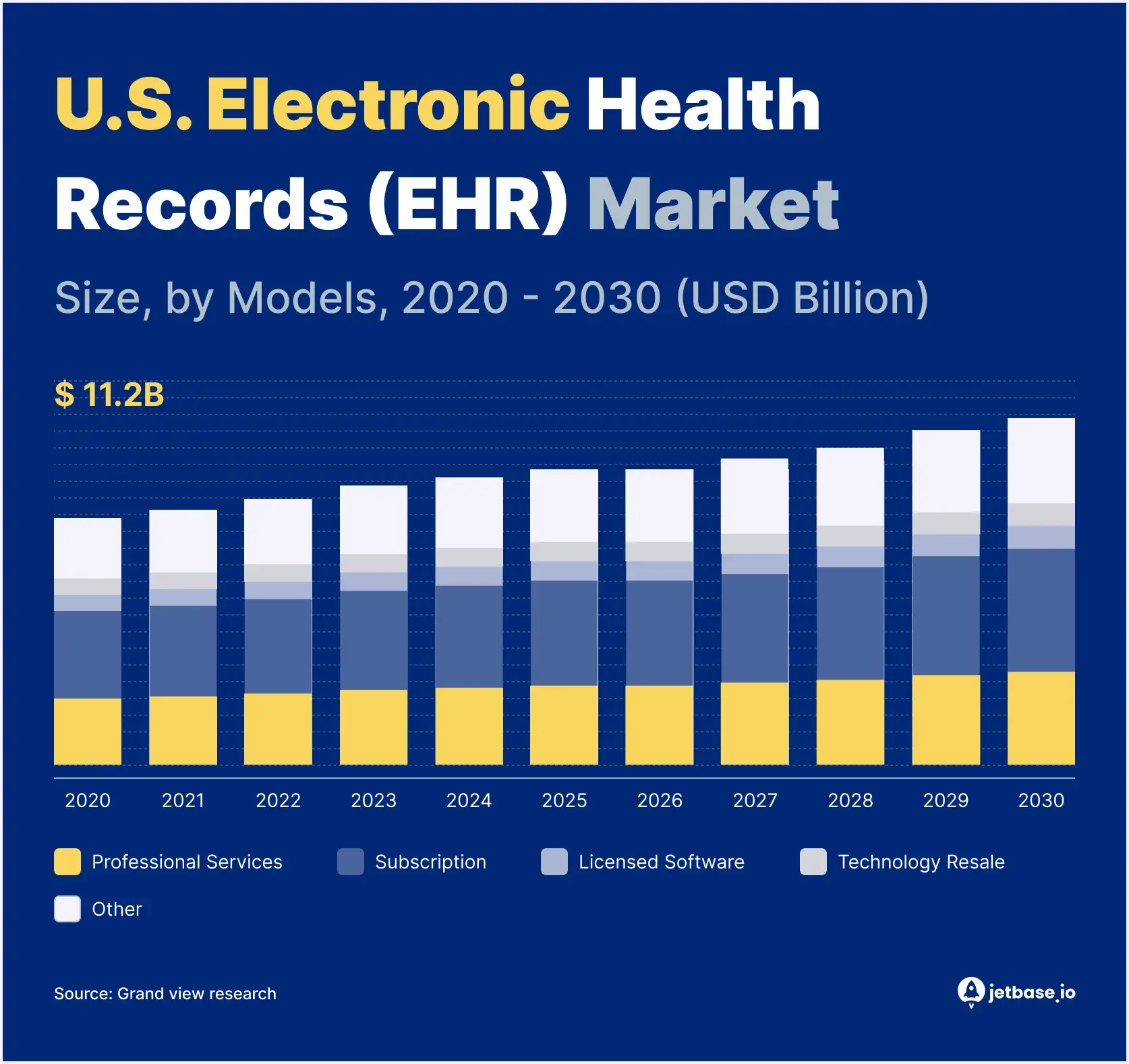
Electronic health records (EHRs) come as a way to store and manage patient data digitally. And, more importantly, streamline workflows and billing. With their global market growing from $29 billion in 2023 to over $38 billion by 2030, you cannot but acknowledge the EHRs’ importance for patients, doctors, and entrepreneurs alike.
Building on JetBase’s previous discussion about healthcare software development, let’s explore a specific type — EHR systems. Read on to discover the essential features they should have, the benefits they offer, and the challenges you might face. Most importantly, you’ll learn the core steps for building an EHR system in 2025.
What Is an EHR System?
An EHR system is software that stores a patient’s entire medical history. The information it usually contains (but isn’t limited to) includes the following:
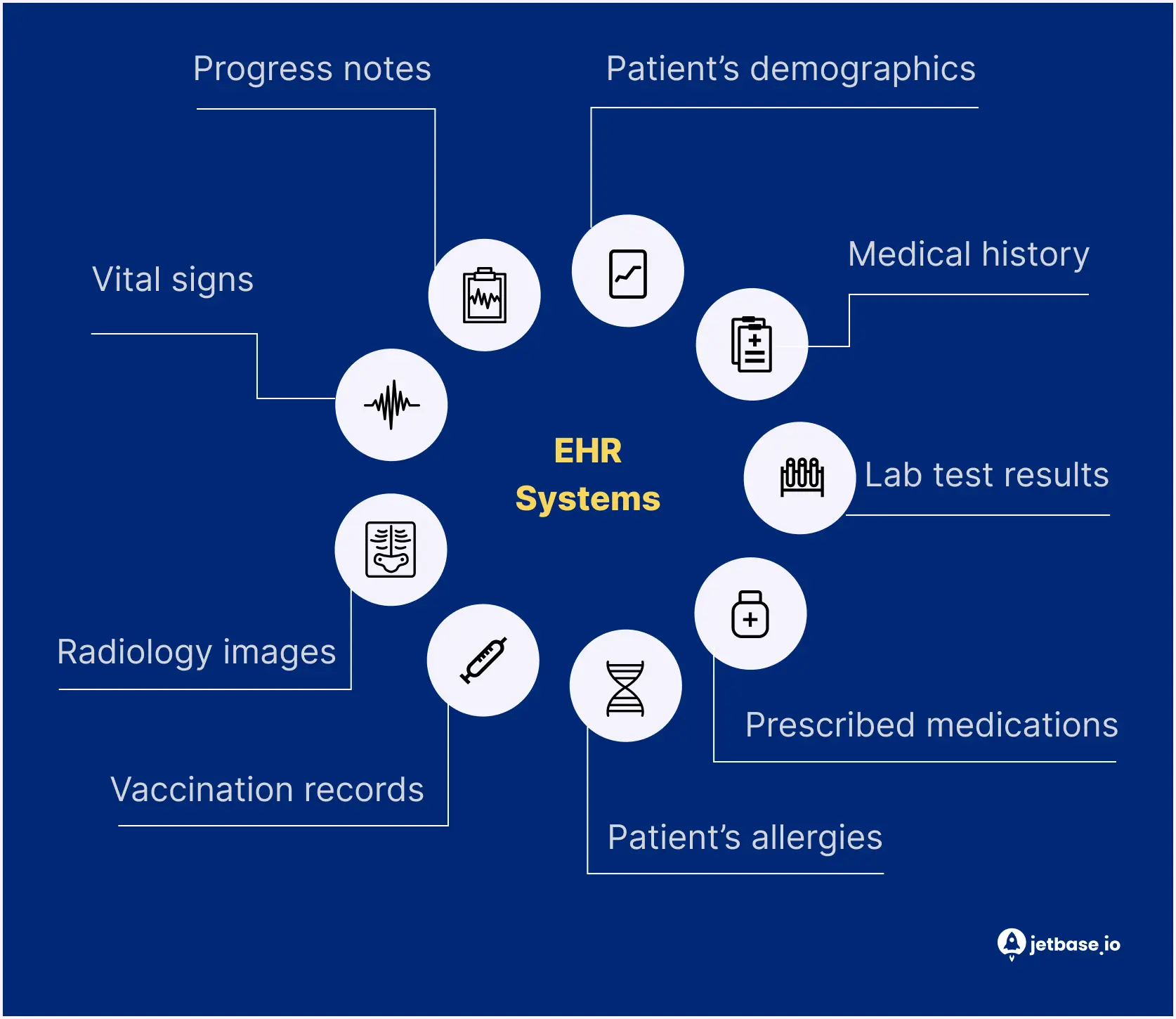
The EHR system lets any authorized individual involved in a patient’s care access, manage, and share these records. Hence, doctors, lab administrators, pharmacists, and, of course, patients themselves can leverage EHR.
EHR vs. EMR vs. Practice Management Software: Key Differences
When dealing with EHR system development, you may stumble upon terms like EMR and practice management software. While often used interchangeably, these are different solutions. Let’s explore the distinctions between them:
- Electronic health record (EHR). An EHR provides a comprehensive view of a patient’s health and combines data from various sources (labs, pharmacies, hospitals, and so on). It focuses on patient-centered care and includes information beyond a specific healthcare provider’s office.
- Electronic medical record (EMR). Compared to an all-around EHR, an EMR system contains a patient’s history within a specific healthcare organization. Consider it a digital version of a regular paper chart that doesn’t integrate data from external sources.
- Practice management software. In contrast to EHRs and EMRs that handle the clinical part of the healthcare organization, practice management software covers administrative tasks. It typically features appointment management, billing, and insurance claims and may or may not integrate with EHR or EMR systems.
Types of EHR Systems
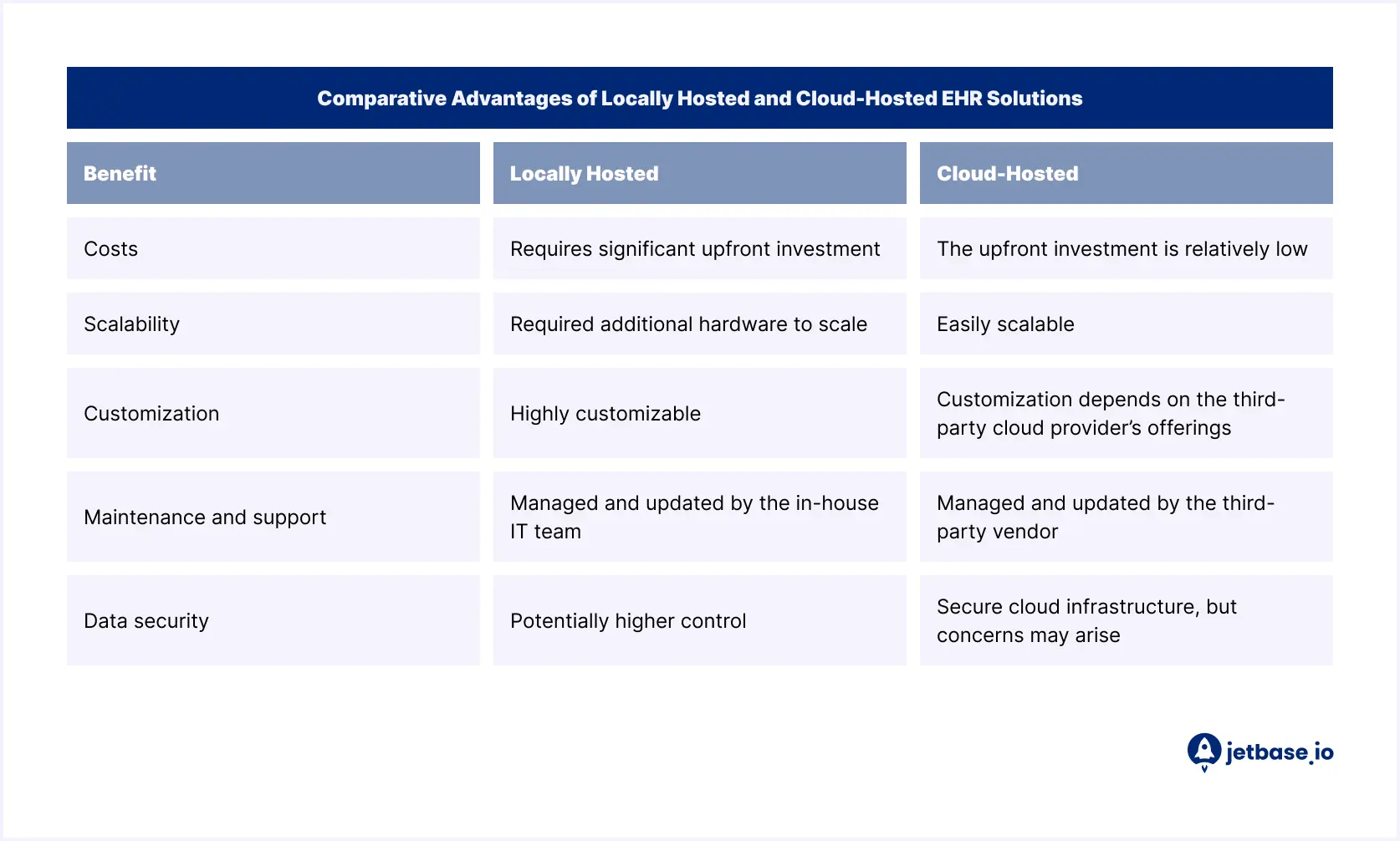
There are two main types of EHR systems: locally hosted and cloud-hosted. Before starting EHR development, choose which type suits your requirements best. Consider several factors: budget, IT infrastructure, and desired level of control. Here is an overview of both types to help you make a choice.
Locally Hosted vs. Cloud-Hosted EHR Solutions
Based on the deployment model, there are two types of EHR solutions:
- Locally hosted. Also known as on-premise solutions, these EHR systems are installed and maintained on local servers at the healthcare provider’s office. In this approach, the in-house IT team manages and updates the hardware, software, and security infrastructure.
- Cloud-hosted. These EHR solutions use remote servers and infrastructure managed by third-party cloud service providers (e.g., Google Cloud, Microsoft Azure, Amazon Web Services). Healthcare practitioners access the system through the Internet without worrying about local hardware or software installation and maintenance.
Comparative Advantages of Locally Hosted and Cloud-Hosted Solutions
Selecting the right deployment model depends on your specific needs and priorities. Let’s review the benefits of each EHR solution, locally hosted and cloud-based:
Core Benefits of EHR Software
Building an EHR system is more than just creating a single source of truth for patients, doctors, and healthcare facilities. It’s also about making the lives of all stakeholders easier through the following perks:
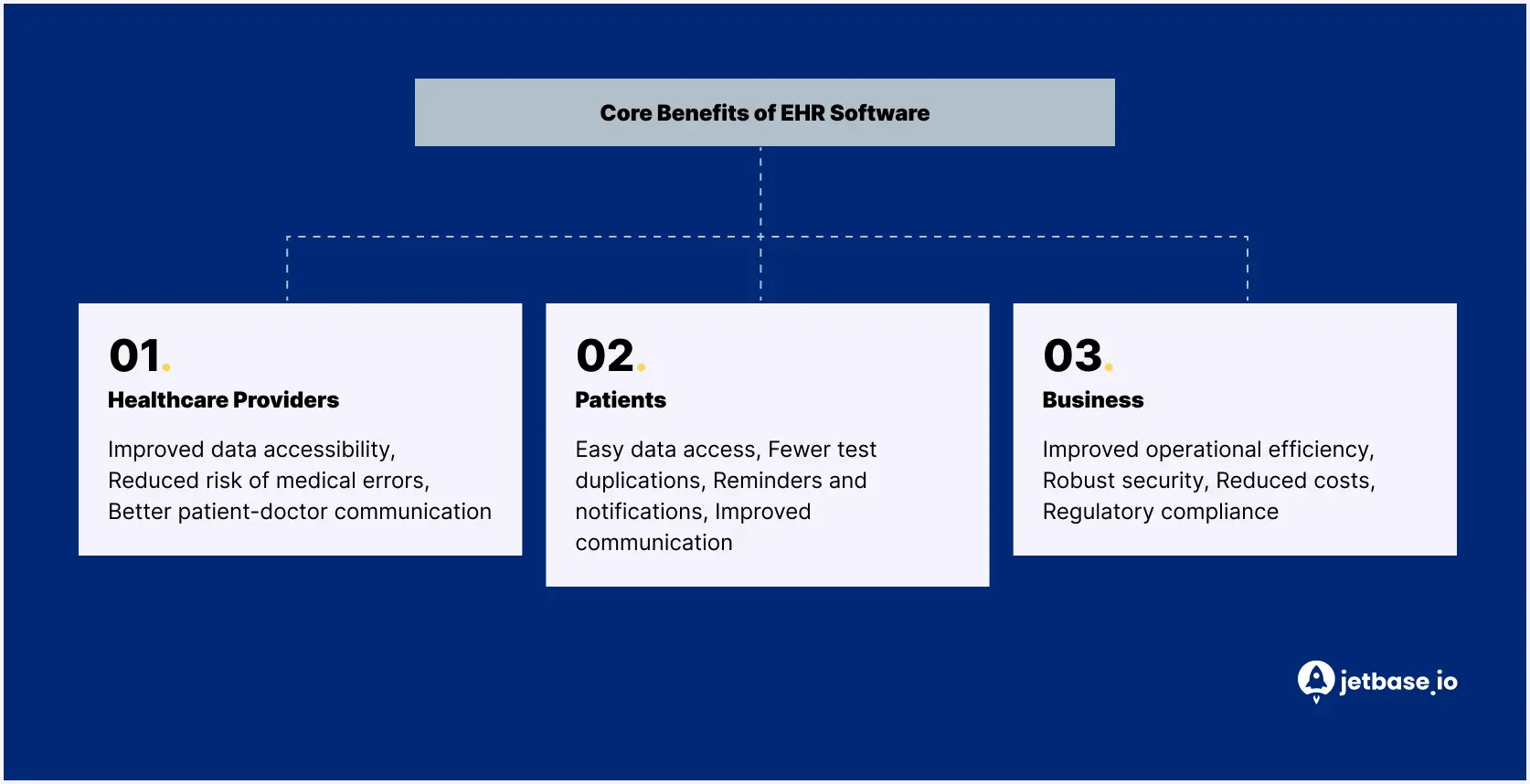
Benefits for Healthcare Providers
Here’s how doctors and other medical personnel benefit from EHR software development:
- Improved data accessibility. EHRs let healthcare providers access patient records instantly without needing to search through piles of paper charts. As a result, doctors can deliver patient care faster and more precisely.
- Reduced risk of medical errors. By having all the necessary patient data at their fingertips, healthcare professionals make better treatment decisions. They can check drug interactions, allergies, and other adverse reactions the patient might have to avoid incorrect prescriptions and other mistakes.
- Better patient-doctor communication. EHRs facilitate interactions between patients and healthcare providers through features like appointment booking, messaging, and seamless data exchange.
Benefits for Patients
With EHR solutions, patients get a more complete picture of their health and plenty of other advantages:
- Easy data access. Patients can view their test results, medications, vaccination records, and treatment plans online through dedicated patient portals, which gives them more involvement in their own healthcare decisions.
- Fewer test duplications. EHR systems help prevent duplicate tests by recording past tests performed. This saves patients time and money and eliminates unnecessary discomfort.
- Reminders and notifications. EHRs can send patients appointment reminders, medication refill alerts, and other treatment notifications.
- Improved communication. EHR solutions let patients communicate with their healthcare providers easily and receive timely care or support for chronic disease treatment.
Business and Operational Benefits for Medical Practices
Besides just patients and doctors, EHR solutions benefit entire hospitals and medical practices. The advantages are as follows:
- Improved operational efficiency. EHR systems usually include appointment scheduling, billing, and reporting features. This way, hospitals automate tasks and free up staff time.
- Robust security. EHRs typically leverage strong security measures like multi-factor authentication, digital signatures, encryption, and access controls. This ensures a high level of data protection.
- Reduced costs. EHR development is cost-effective in the long run. Using EHRs lets hospitals save costs through reduced paperwork, improved billing efficiency, and lower error rates.
- Regulatory compliance. EHRs standardize documentation and reporting, ultimately ensuring compliance with different healthcare regulations.
Essential Features of an Effective EHR System
Learning how to create EHR software requires thinking about the functionalities you need. Features may differ from system to system, but there are several ones you cannot miss:
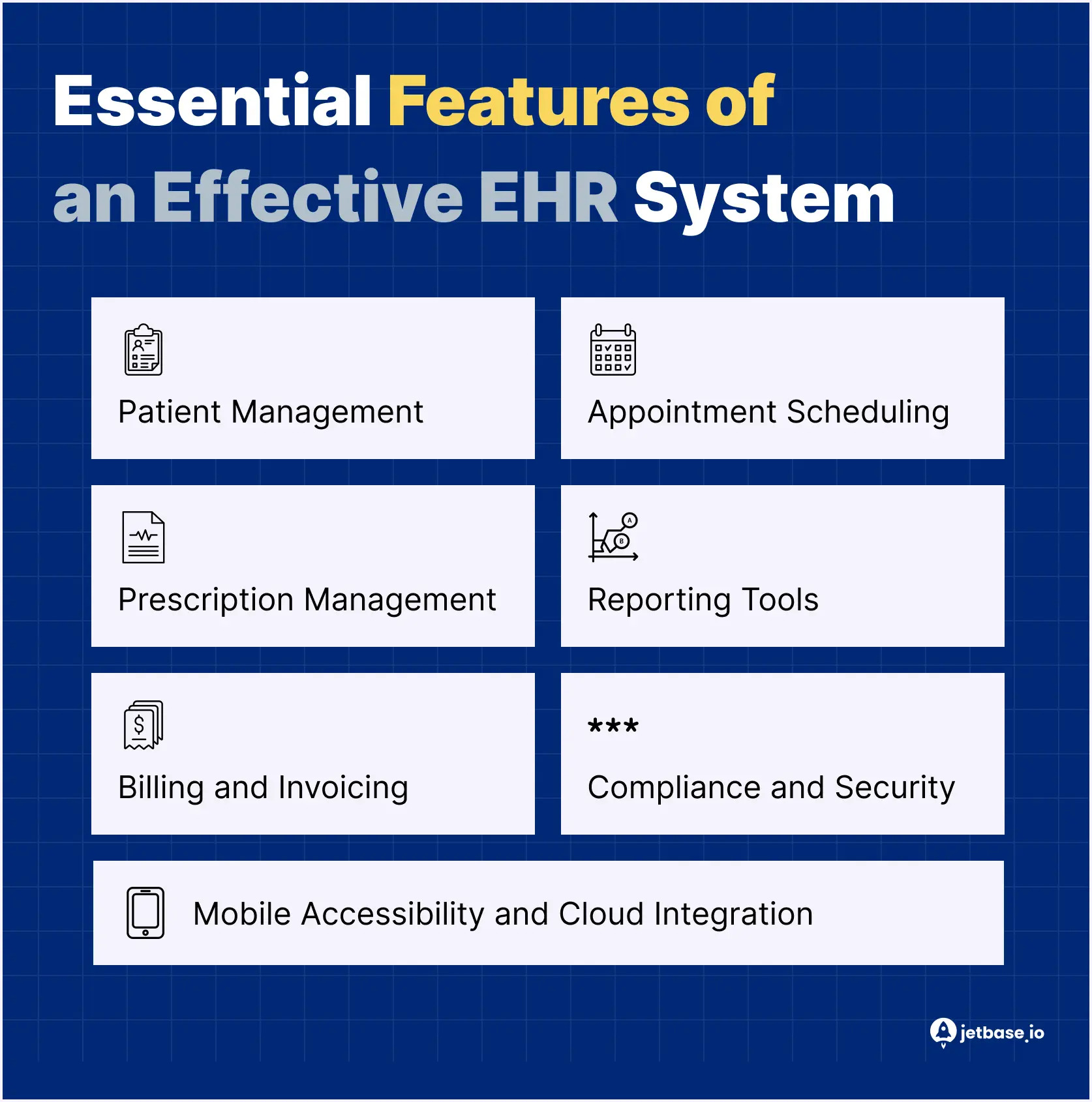
Patient Management
Patient management functionalities let healthcare providers create and maintain electronic records for each patient. This feature is twofold and comprises the following:
- Patient records. These store a patient’s medical history, including demographics, allergies, medications, lab results, and so on.
- Patient portal. This platform allows patients to view their medical records, schedule appointments, request medication prescriptions, and connect with their doctors directly.
Appointment Scheduling
Appointment scheduling lets patients book appointments with their doctors through the EHR system itself or a patient portal. Usually, this feature comes with automatic appointment reminders.
On the healthcare professional’s side, this functionality enables appointment management: scheduling, rescheduling, or canceling.
Prescription Management
Prescription management enables the following:
- Electronic prescribing (e-prescribing). Healthcare professionals prescribe medicines to patients online and transfer the prescriptions to pharmacies.
- Drug interaction checks. Doctors can review patient data and run drug interaction checks to ensure patient safety.
- Refill management. Patients can request medication refills online.
Reporting Tools
Reporting is an essential feature for both healthcare providers and patients.
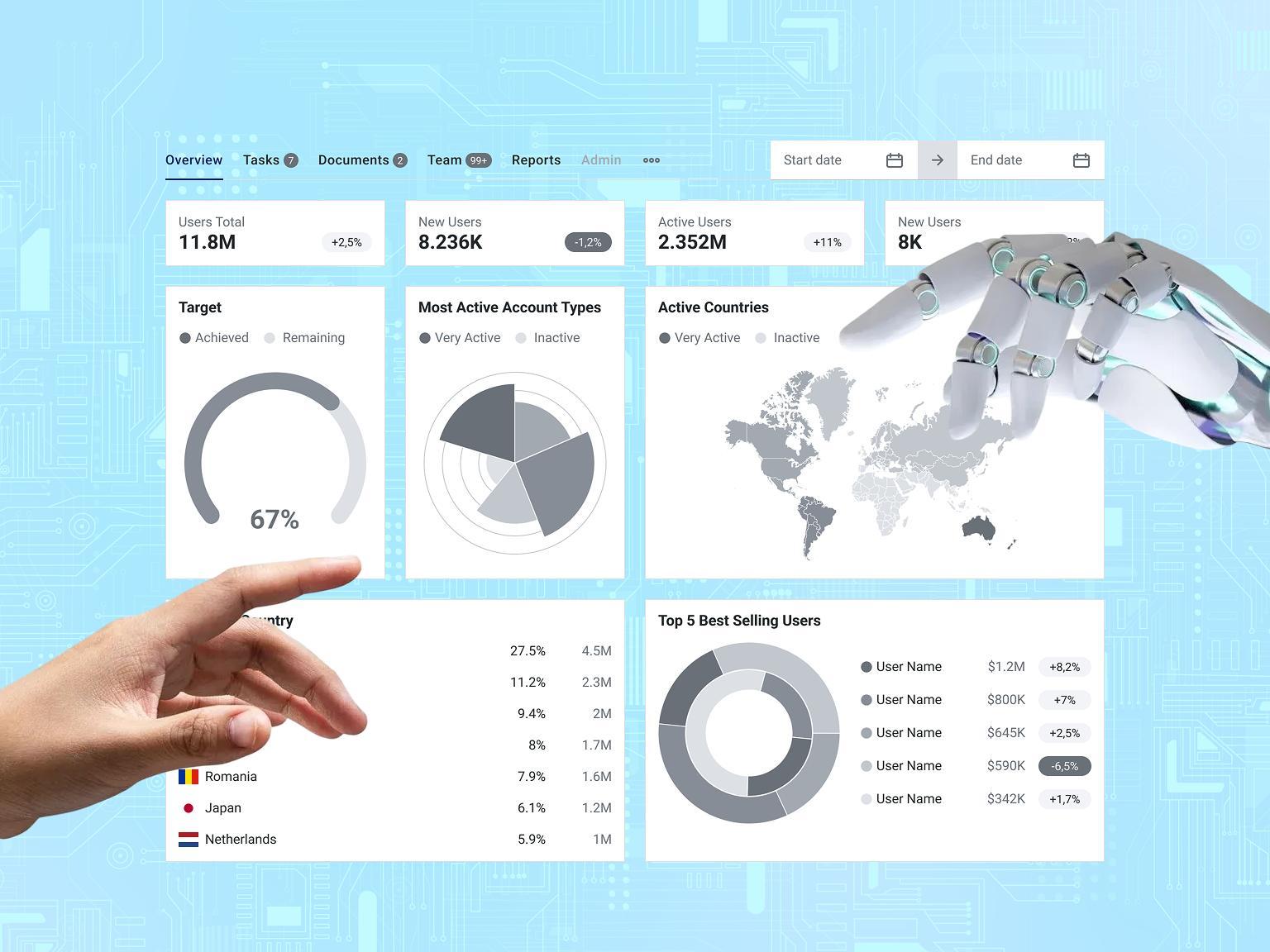
By leveraging reporting tools, healthcare organizations get a comprehensive view of patient data, quality of treatment measures, and practice performance. They can also analyze this data to suggest improvements in patient care.
Patients, in turn, get a visual representation of their treatment plans, scheduled hospital visits, and beyond.
Billing and Invoicing
EHR software development is simply impossible without billing and invoicing features. Hospitals and healthcare professionals demand the tools necessary for simplifying payments. Some of those may include:
- Billing. This allows for the creation and submission of claims.
- Invoicing. This tool lets you generate and send invoices to patients.
- Payment processing. EHRs may integrate with online payment processing systems for patient payments.
- Insurance verification. This enables verification of patient insurance coverage.
Compliance and Security
Compliance and security ensure adherence to regulatory requirements and patient data safety. Role-based access controls, encryption, multi-factor authentication, digital signatures, and regular security audits are examples of protection measures. Following HIPAA, GDPR, and other regulations guarantees patient information privacy.
Mobile Accessibility and Cloud Integration
Mobile accessibility allows healthcare providers and patients to access an EHR system anytime, anywhere. This requires building a dedicated mobile app or an EHR platform that supports mobile devices. The app may gather and analyze data from health-tracking devices to monitor various parameters such as heart rate, steps, calories burned, sleep patterns, blood oxygen saturation, electrocardiogram (ECG), body temperature, hydration levels, etc. Hosting an EHR system in the cloud offers scalability, flexibility, and cost-effectiveness.
How AI Enhances EHR Functionality
EHR systems are undergoing a transition in provider interaction through artificial intelligence implementations. The integration of AI features would enhance your solution through these functions:
- Predictive analytics analyzes patient records through AI to predict medical issues that may occur or recommend timely preventive measures.
- The Natural Language Processing tool of NLP transforms doctor voice remarks into structured patient information in smart charting functions.
- The system automatically identifies irregular patterns or medication omissions thus enhancing patient results.
- The system features clinical decision support through which artificial intelligence powered tools present treatment recommendations based on patient history combination with symptoms data.
The system's capabilities help to cut down on clinical work while enabling rapid precise judgments which become especially important in urgent situations.
Building an EHR System: A Step-by-Step Guide
Now that you know the essential EHR features, it’s time to explore the main thing: how to develop EHR software. JetBase prepared a detailed breakdown of the steps involved:
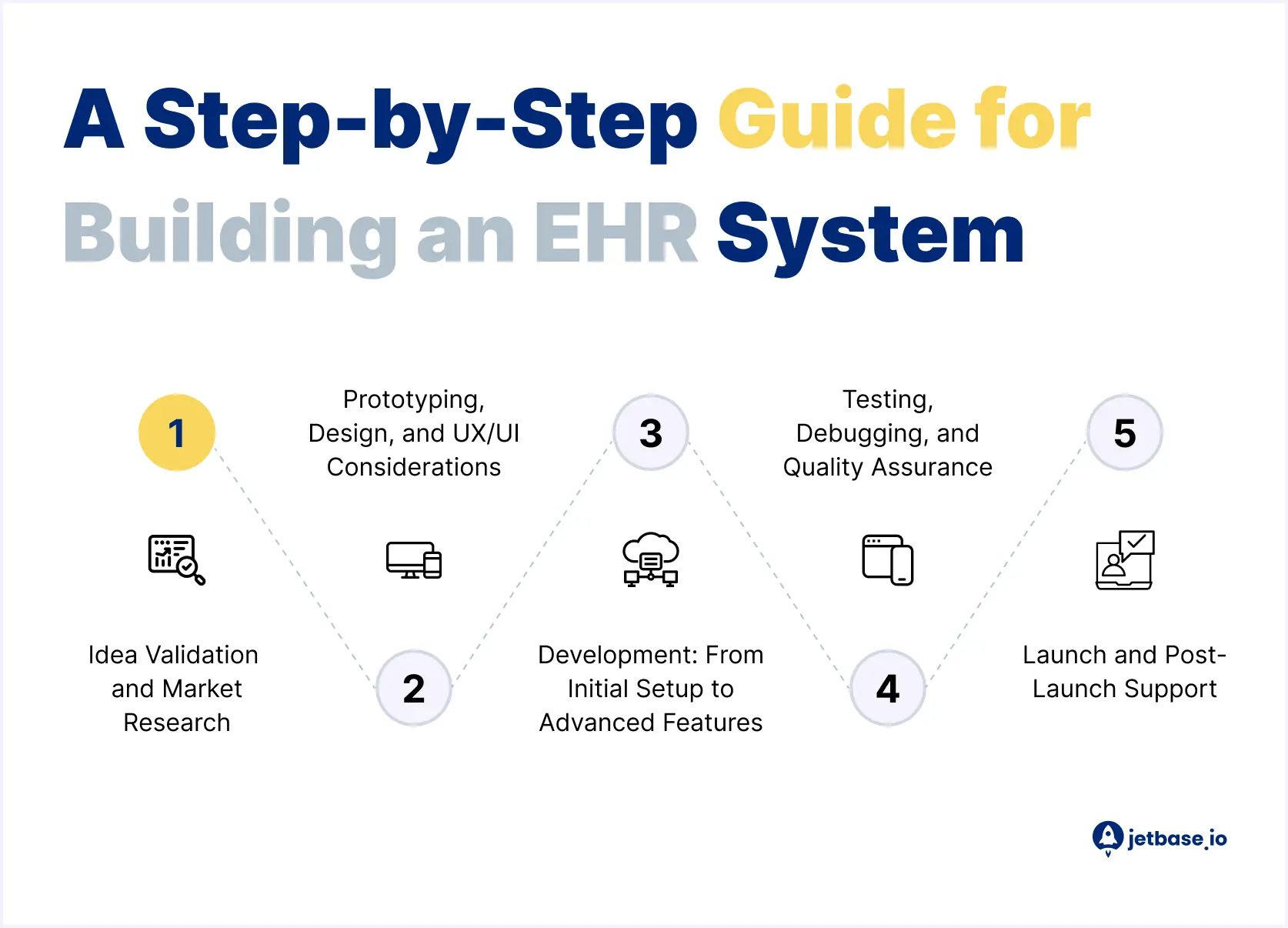
1. Idea Validation and Market Research
Before the actual EHR system development, you should validate your idea and handle thorough market research.
First, define your niche. You might assume that creating an EHR system already determines your niche. However, the EHR market is vast, and so is your potential audience.
Then, do the following checks:
- Research existing solutions and identify a specific niche or unmet need your system can address.
- Determine the healthcare organization’s size for which you’re building the software.
- Focus on a clear target audience.
- Research your competitors and their strengths and weaknesses.
- Evaluate the overall market size and growth potential for your solution.
- Conduct interviews and surveys with potential users to gather feedback on their pain points and desired features.
After that, you must have a clear understanding of your niche, target audience, and competitive advantage.
2. Prototyping, Design, and UX/UI Considerations
Once you’ve validated your EHR system idea, proceed to prototyping. As part of this process, cover the following:
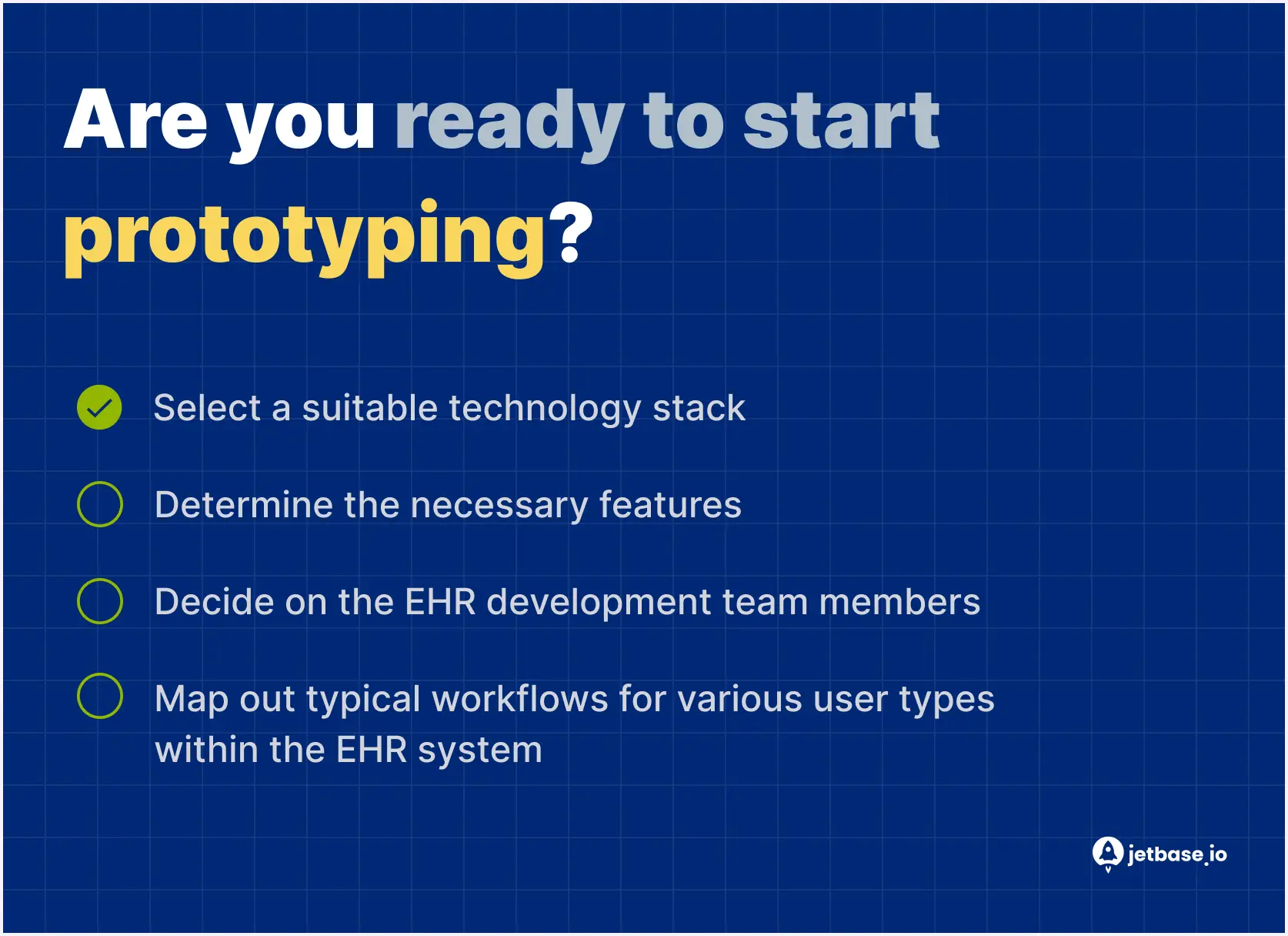
Then, create prototypes to visualize the system’s functionality and user interface. Gather user feedback on the prototypes to improve the design.
With a ready-made prototype, move to your EHR system’s UX/UI design. Create wireframes and user journeys that will be seen in your software’s final version. Design with usability, accessibility, and intuitive navigation in mind.
3. Development: From Initial Setup to Advanced Features
EHR software development can be broken down into several phases. Here’s how to build an EHR system gradually:
- Initial setup. Establish the infrastructure locally or leverage the cloud-based model.
- Core functionality development. Implement essential features like patient management, appointment scheduling, prescription management, and others.
- Third-party systems integration. Integrate your EHR with existing lab results systems, pharmacies, and other relevant healthcare software.
- Advanced functionality development. Consider implementing advanced features like clinical decision support, messaging, and beyond.
- Security and performance. Introduce security measures, ensure regulatory compliance, and optimize code for efficient EHR system operation.
4. Testing, Debugging, and Quality Assurance
Handle various types of testing to identify bugs and flaws in your EHR system before launch. Conduct unit, integration, system, security, and user acceptance testing.
Fix the bugs you’ve found through thorough debugging and quality assurance processes. Make sure your system follows the necessary regulations and data security standards throughout the testing phase.
5. Launch and Post-Launch Support
Work on the launch plan for your EHR system. To market your software successfully, consider:
- Developing training materials and providing ongoing support to users to ensure they use the system effectively.
- Establishing a marketing strategy to reach your target audience.
- Migrating existing patient data from previous systems to your new EHR if necessary.
After you launch your EHR software, take care of ongoing maintenance and support. Ensure regular bug fixes and updates to keep your system relevant.
 Compliance and Certification in EHR Software Development
Compliance and Certification in EHR Software Development
As we’ve already mentioned, regulatory compliance is a must in EHR software development. Here are the considerations you should pay attention to:
HIPAA Compliance

The Health Insurance Portability and Accountability Act (HIPAA) is the legislation that ensures the protection of patient health information in the United States. There are 75 security protocols your software must comply with under HIPAA.
Generally, to follow this regulation fully, you must address the following:
- Ensure security measures to protect patient health information. This includes strict access controls, security audits, and encryption.
- Guarantee health information privacy and let patients access, modify, and request reporting of disclosures of their data.
GDPR and Other Regulatory Considerations

Besides just HIPAA, which operates within the US, you may need to comply with other regulations that cater to such regions as the European Union. In this case, ensure compliance with the General Data Protection Regulation (GDPR). This law has stronger consent requirements compared to HIPAA.
On top of that, make sure your EHR system follows HL7 — international standards for data sharing between healthcare providers.
Achieving Certification for EHR Systems
A custom EHR system must also adhere to certain industry standards. One such is a certification from the Office of the National Coordinator for Health Information Technology (ONC HIT) in the US. This program ensures that EHR systems meet specific interoperability, security, and functionality criteria.
The EU-based systems must obtain the EuroRec certification, which is similar to ONC HIT.
Interoperability and HL7/FHIR Standards
An EHR system needs interoperability features to enable smooth data exchange between healthcare providers. HL7 and FHIR provide the standards needed for this purpose.
- The messaging standards used for health data exchange between systems are defined through HL7 (Health Level 7).
- Healthcare organizations use FHIR (Fast Healthcare Interoperability Resources) which provides a web-based standard to speed up and enhance data sharing capabilities.
The implementation of these standards guarantees your system will function through these capabilities:
- The system must exchange data with laboratories as well as hospitals and pharmacies.
- Wearable devices together with telemedicine apps become accessible through the system.
- Multiple electronic platforms should provide patients access to their medical records to view and manage them.
Cost Analysis of Developing an EHR System
Building an EHR system requires substantial investment, and the final price typically relies on:
- The complexity and number of features.
- The chosen development approach, whether in-house dev team, outsourcing, or a freelance EHR developer.
- The size and location of your development team.
- The tech stack used for the EHR system.
- The infrastructure costs.
Let’s estimate the approximate price of an EHR solution, given the average outsourcing rate of $50. Here are the processes involved in development, their timelines, and costs:
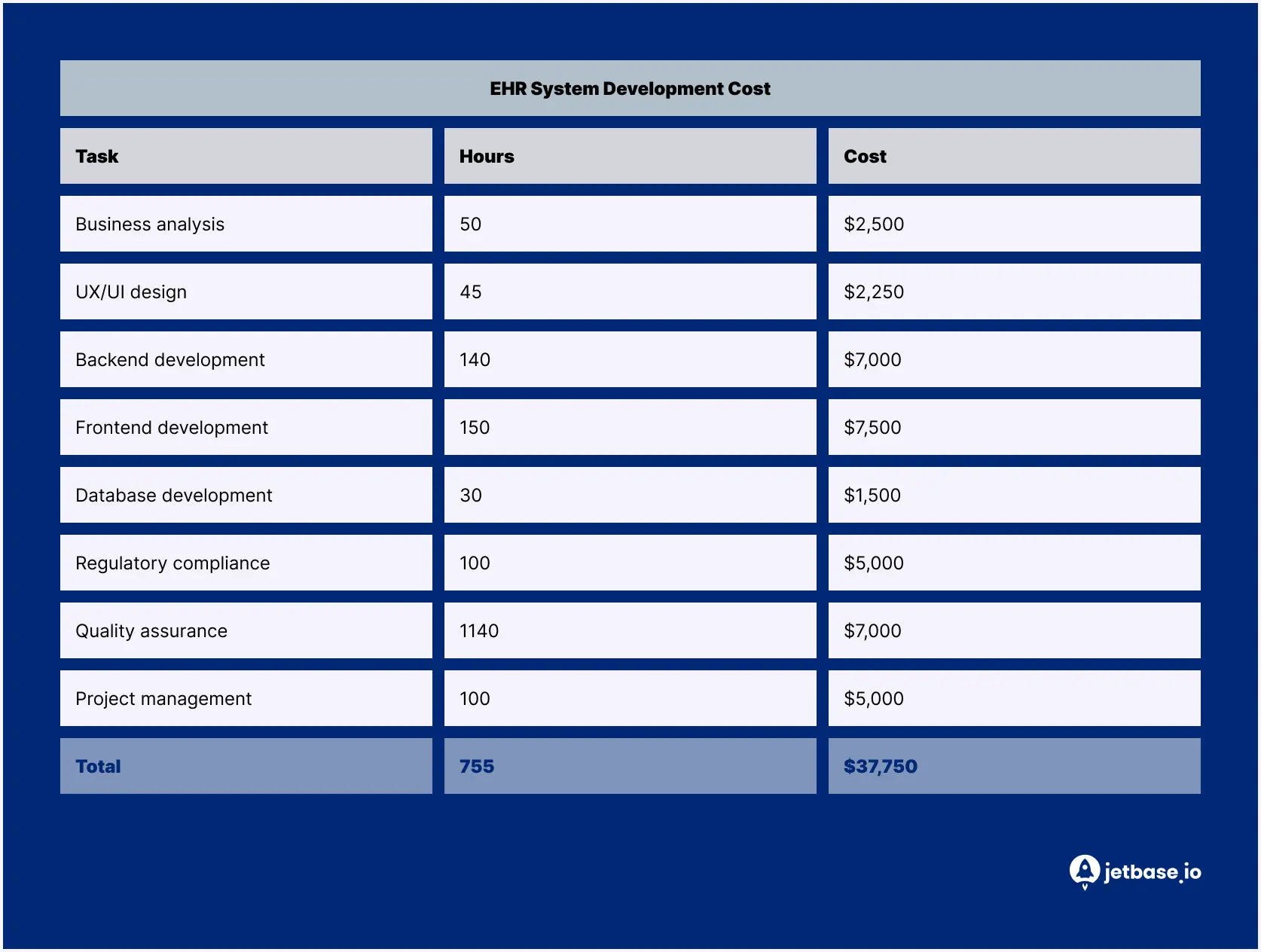
However, these are just estimates. To get a more accurate picture, reach out to JetBase experts.
Choosing a Development Partner for Your EHR System
Learning how to create an EHR system is a complex task. Therefore, it’s best to delegate development to professionals. But how do you know if your dev partner is “the one”? Here are several tips:

Alternatively, skip the above tips and choose to partner with JetBase. How can we help?
We have over 5 years of experience in healthcare software development and 10 years of experience in software development. Therefore, our team is familiar with security measures, relevant regulations, and technologies used in EHR systems. We can build EHR software from scratch, update the legacy solution, or integrate EHR into your existing platform. Contact us today for a free consultation and a more accurate estimation.
For example, when our team worked on the healthcare mobile app, we had to enable remote patient monitoring. To achieve this, we introduced reminders that encouraged regular health check-ups via connected devices and allowed doctors and patients to access and compare health data. We also featured:
- Health measurement history.
- Medication tracking.
- Data exchange between patients and doctors.
As a result, we delivered a product that simplifies health management and enables seamless data sharing for all parties involved.
For more insights into our experience, feel free to check out our portfolio.
Common Challenges and Solutions in EHR Development
Building an EHR system isn’t as straightforward as it may seem. During the process, you may face certain challenges and limitations. But the good news is there’s always a solution.
Technical Challenges and How to Overcome Them
On the technical part of EHR software development, you may struggle with the following:
- Security implementation. EHR systems contain sensitive patient data, which makes them vulnerable to cyberattacks. To mitigate the risks of data breaches, introduce role-based access controls, data encryption, multi-factor authentication, and other measures.
- System integration. EHR software frequently requires integration with pharmacies, laboratories, and other vendors. To facilitate smooth connection, rely on the HL7 standard and make sure your development team has relevant expertise in healthcare data integration.
- Scalability. Eventually, your EHR system will need to handle larger loads. Therefore, build your software with scalability in mind. Consider a cloud-hosted solution that can accommodate increased traffic and data storage requirements.
User Adoption and Training Best Practices
Other obstacles are related to the end-users of your EHR system. Here’s what you’ll potentially have to deal with:
- Resistance to change. Some healthcare providers may hesitate to adopt a new EHR system, especially if they’re comfortable with what they already use. To pique their interest, offer detailed training materials and provide support along the way. Gather feedback and solve any occurring usability issues right away.
- System complexity. EHR software can be too complex for a regular user. That’s why focus on user-friendliness. Make the interface intuitive and easy to navigate for users with different levels of technical expertise.