In the healthcare insurance industry, where modern technologies like AI, big data processing, and machine learning are rapidly being adopted, there remains a significant reliance on manual processing. Companies continue to hire people instead of robots for tasks such as registration, billing, claims, and other insurance-related processes.
But are automated systems really inferior to human workers? Is automation worth implementing? This question is a double-edged sword. In this article, we'll explore a case from our practice at JetBase, where we successfully replaced human labor with automated billing processes, benefiting everyone involved. Rest assured, no one was fired; instead, everyone gained from this transition.
Keep reading to understand how insurance automation can streamline and enhance workflow efficiency.
Understanding Patients' Insurance Conditions
Proof of treatment is a crucial component in the healthcare insurance ecosystem. It is an essential condition of the policy or contract between the insured and the insurer.
Typical Conditions in a Health Insurance Policy
| Pre-Loss Conditions |
|
| Ongoing Conditions |
|
| Post-Loss Conditions |
|
| Financial Conditions |
|
| Special Conditions |
|
Proof of treatment can include doctor prescriptions, clinic bills, or other medical records. The accuracy and timely provision of these documents are crucial. However, many cases arise where representatives of medical billing management lose documents due to the high volume of data, poor management system, or human error.
This is where automation comes in. It aims to reduce manual workflow during billing and claim processing, policy updating, and other insurance-related tasks.
How Automation in Healthcare Insurance Works: A Case Study
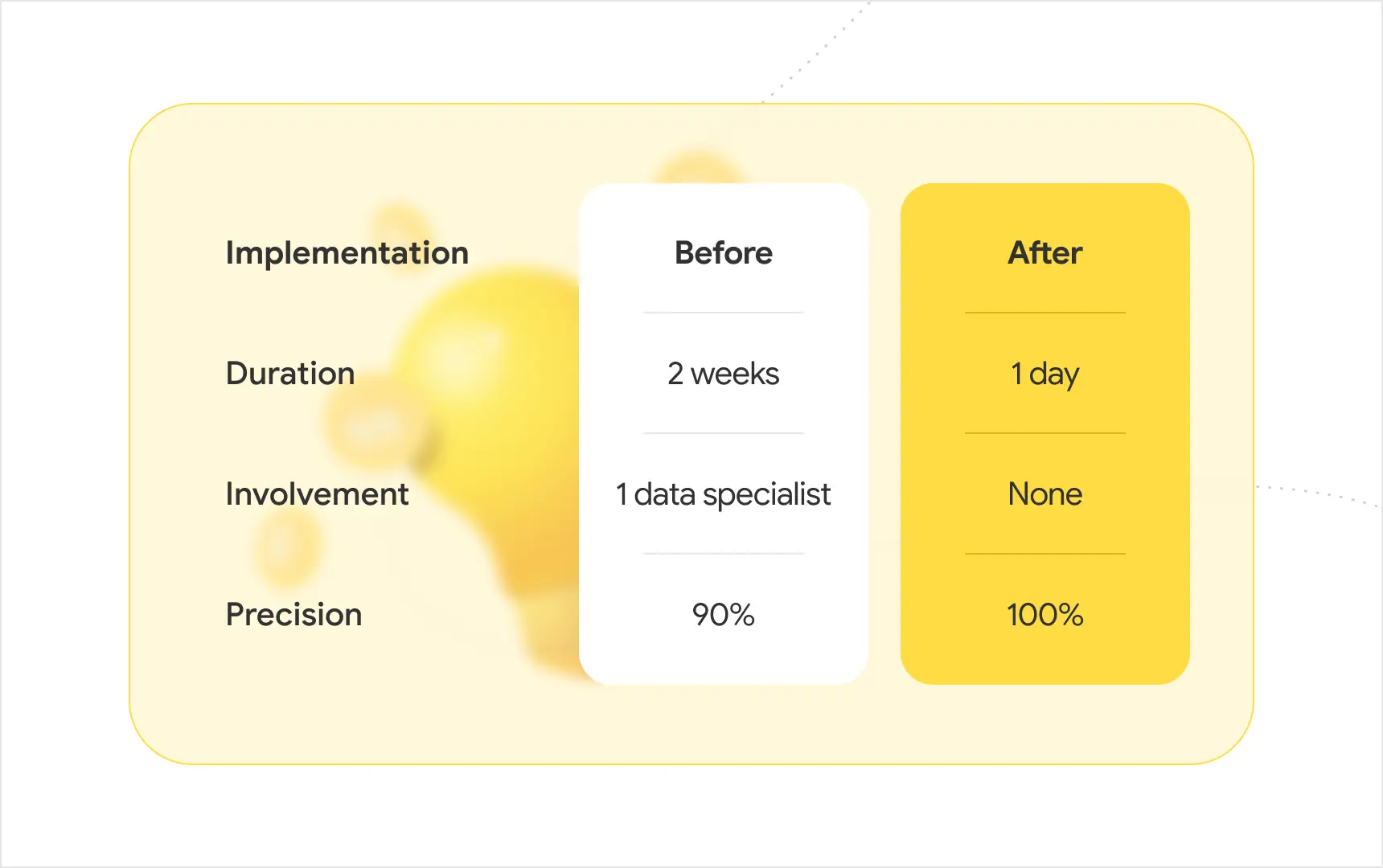
To illustrate how automation works, let's present a case study where we reduced billing data processing time from two weeks to one day.
Data Processing Time for Billing Automation
Data Utilized
In our case study, the data processed includes doctors' time spent on patient records. This time is recorded in seconds, and once it reaches about 20 minutes (1200 seconds), the system assigns a Current Procedural Terminology (CPT) code. These codes provide a standardized nomenclature for coding medical procedures and services.
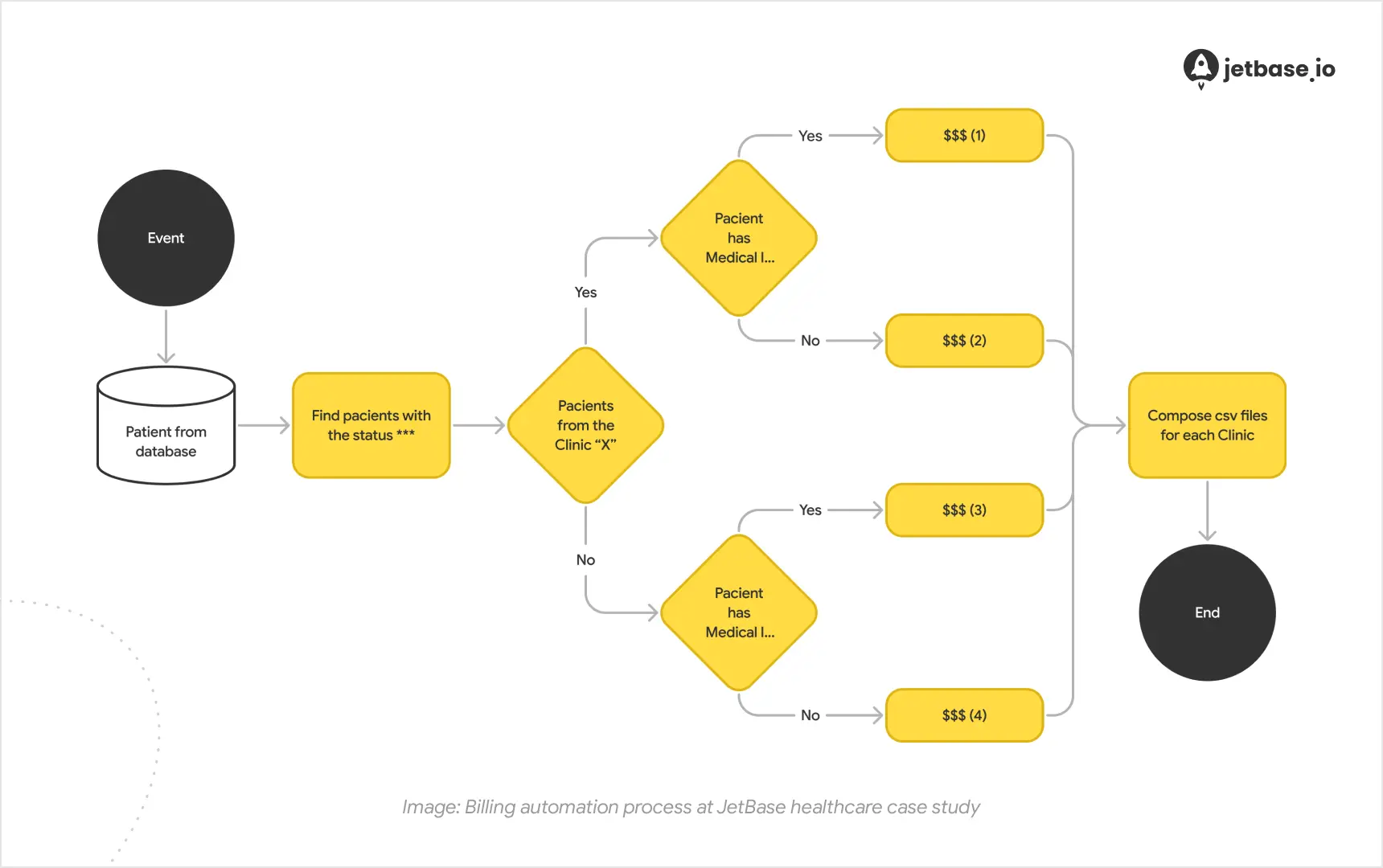
The insurance company receives reports containing these codes and the patient's treatment history, including calls, consultations, and medical prescriptions. Accurate coding is crucial for billing, and before automation, a dedicated manager manually calculated thousands of codes, taking weeks and requiring multiple rounds of verification.
With automation, this person transitioned to other tasks, eliminating the need for manual documentation processing.
Ensuring Data Reliability
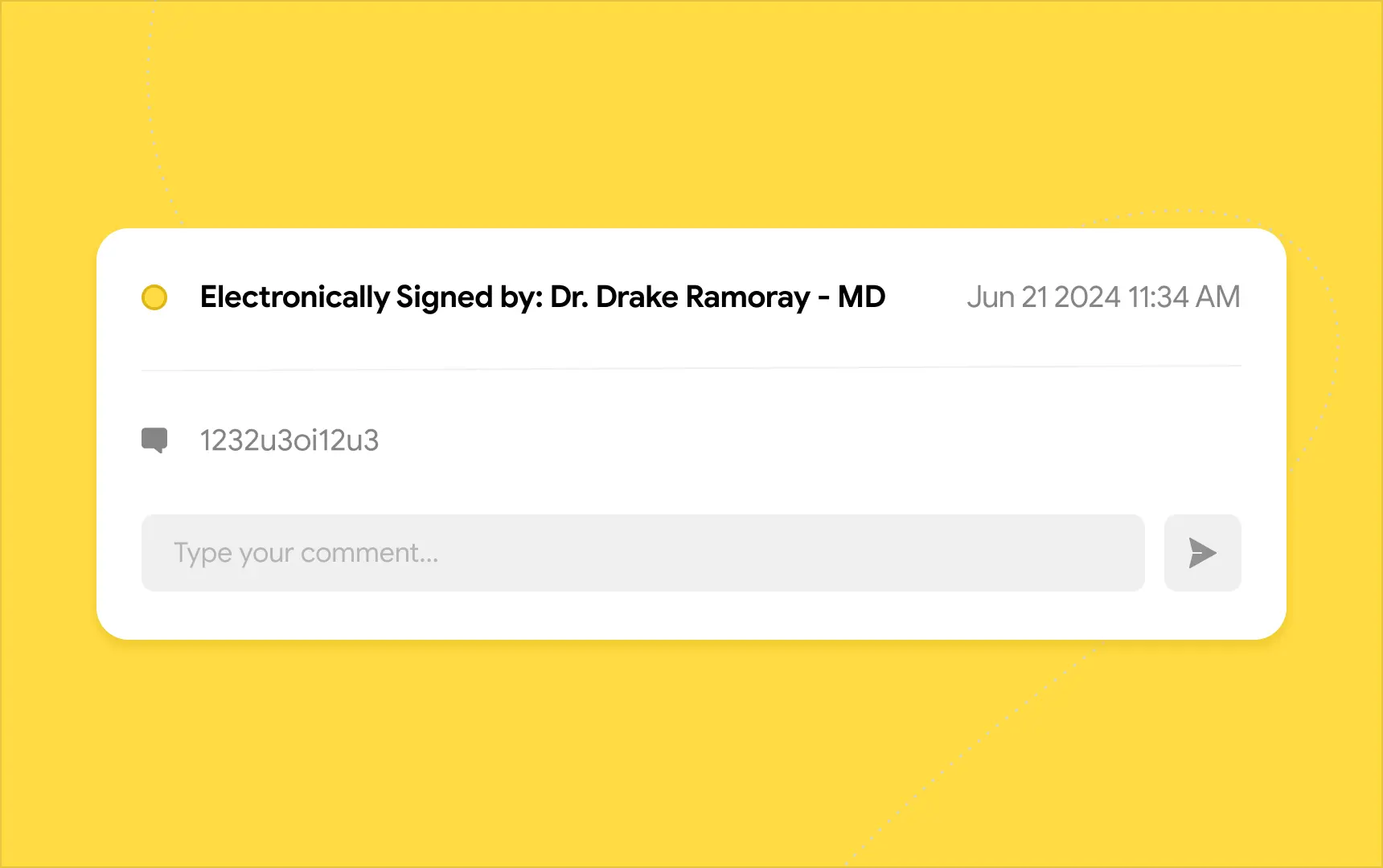
Ensuring the accuracy of all data is critical. Our responsibility includes verifying that recorded work hours match reality, requiring human oversight. We implemented electronic signatures for doctors, who must approve interim reports to confirm their accuracy.
Technical Stack for Billing Automation
We chose the most relevant technical services based on our project infrastructure to ensure HIPAA compliance. The project is based on AWS, utilizing Amazon EventBridge Scheduler with Lambda to initiate processes, as well as SQS to queue the processes. Lambda helped us process logical operations and generate Excel reports, while S3 was used to store the Excel reports.
Challenges in Automation
Working with numerous and repetitive data was challenging. Developing a simple algorithm took time for analysis and testing. Integrating data with third-party services was also difficult. However, we overcame these challenges and achieved 100% accuracy. We double-checked initial records after automation against manual data processing, confirming the high accuracy of our approach.
Determining the Need for Automation
Denied healthcare claims cost physicians a lot of money every year — 65% of claims are never resubmitted despite many recoverable denials (Source).
Not all clinics or insurance providers require automation. Manual medical records management is still prevalent. To determine the need for automation, assess the percentage of denied claims and error rates.
If the denied claims percentage exceeds 5%, automation can help by improving real-time eligibility checks and reducing errors.
"Identifying errors in the medical billing process is crucial and the top priority in automation implementation," says Julia, Quality Assurance and Team Lead at JetBase. "Working with big data means that even a small mistake can lead to significant financial loss."
Recommendations for Billing Process Automation
To ensure successful billing process automation, follow these steps:
- Analyze the medical billing process.
- Divide the process into parts.
- Automate each part step-by-step.
- Test and verify.
- Split automation processes into manageable cycles.
- Test and verify again.
- Proceed with the final launch.
Benefits of Billing Process Automation
Automation offers numerous benefits to healthcare practitioners:
- Reduces denied claims.
- Avoids repetitive errors.
- Saves time on report creation.
- Enhances customer satisfaction.
- Eases the workload of practitioners and billing managers.
Conclusion
If you're considering whether to implement automation in the billing process, based on our JetBase experience, the answer is a resounding yes. Automation reduces routine data processing, frees up human resources without sacrificing accuracy, and increases satisfaction for both patients and doctors.
We hope this case study has been helpful. If you have any questions about implementing automation in your healthcare project, please don't hesitate to contact us for a free consultation with our experts.