Most areas of modern healthcare readily use digital tools to help patients and improve care flow. However, some institutions still struggle with remote patient monitoring costs and face the technical challenges of adopting new solutions. Thankfully, it doesn’t have to be a dealbreaker.
In this guide, we will explain the components of RPM expenses and how to manage them. We’ll also discuss different RPM types to ensure we cover various approaches to patient care. Plus, we’ll use JetBase’s experience in healthcare software to illustrate our prowess and back up our expertise.
Ultimately, you’ll come away with new knowledge and a direct line to a team of skilled engineers. So, you’ll be able to understand the cost of remote patient monitoring and create your own solution for that purpose. Let’s begin with some groundwork.
Defining RPM and Its Importance in Modern Healthcare
It’s tempting to center remote monitoring and its importance solely around COVID-19 and its difficulties for traditional patient interactions. Sure enough, that was probably the peak time for RPM use, and it will likely remain the catalyst for this niche’s advances. However, RPM’s potential is much more vast.
The cumulative solutions used to monitor patients’ daily status and recovery help doctors check on more people at once and make the process much more affordable. Plus, RPM tools also come in clutch in emergencies when patients use them to report incidents. RPM software guarantees that every user gets the necessary care by tracking their vital signs.
How RPM is Transforming Patient Care and Healthcare Economics
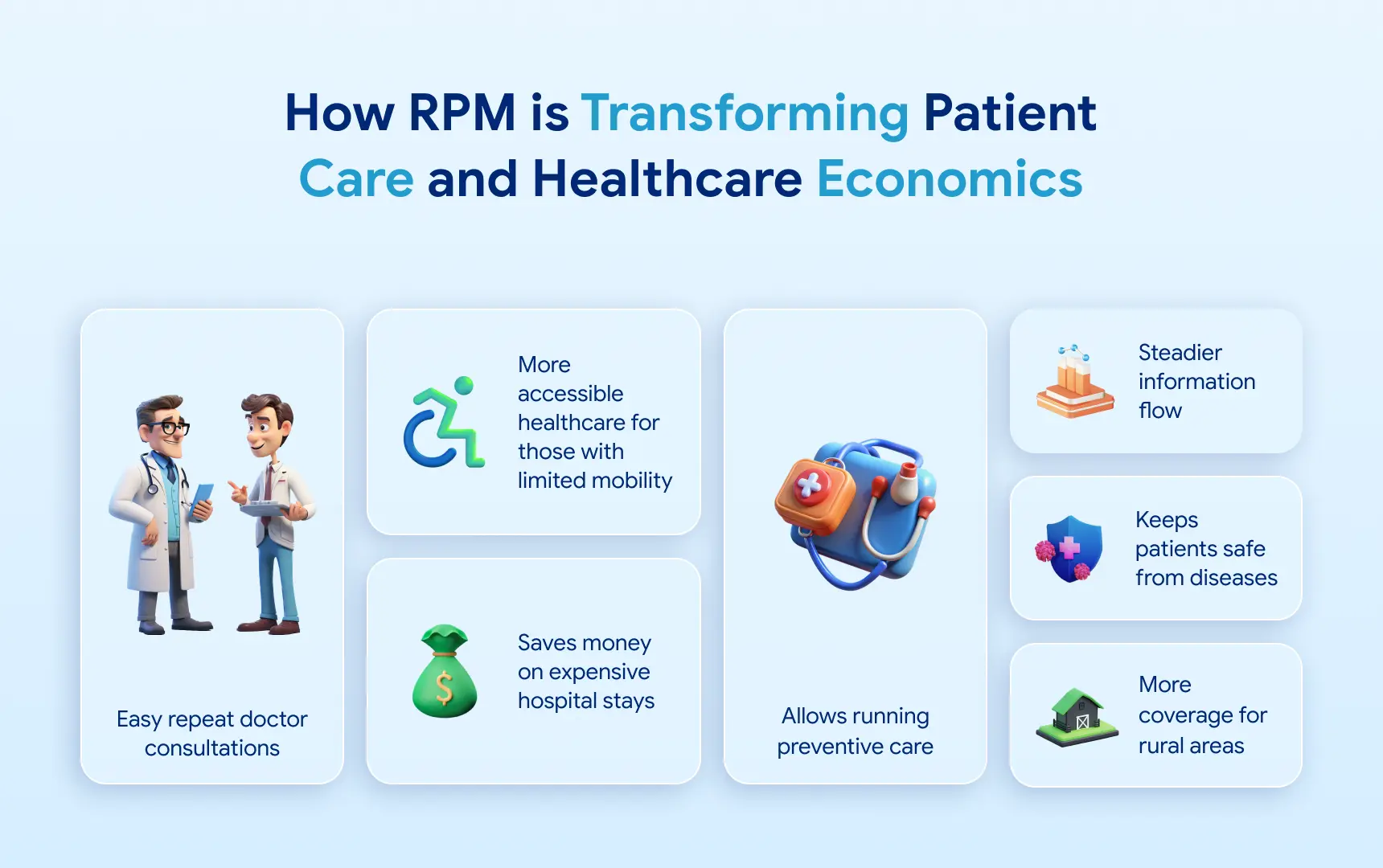
Nowadays, thanks to RPM, it’s easier for a patient to get a doctor’s consultation without paying for repeat consultations, relying on apps instead. Plus, expensive in-hospital stays don’t have to be the norm. Doctors can now survey their patients while they’re cozy in their homes. That also works to keep patients safe from diseases, as shown by RPM research.
While the cost of remote patient monitoring isn’t negligible, it’s still a significant step toward healthcare available to all. Rural areas get better coverage, and those with limited mobility don’t have to go through the hassle of visiting the hospital. Besides, data proves that RPM can be cheaper than traditional methods with a per-patient reduction of $11,472.
Moreover, RPM provides a much steadier information flow, which improves diagnosing and care. Thanks to automated analysis, doctors spot changes in their patients’ conditions early or notice small shifts. As a result, it’s easier to run preventive care instead of playing catch-up as a patient’s state deteriorates.
Types of RPM Software and Their Cost Implications
Despite our use of terms like remote patient monitoring pricing, RPM isn’t a singular thing. It’s the purpose of different software types, each associated with specific uses and benefits. We’ll talk briefly about each of them to give you an idea of this healthcare sector.
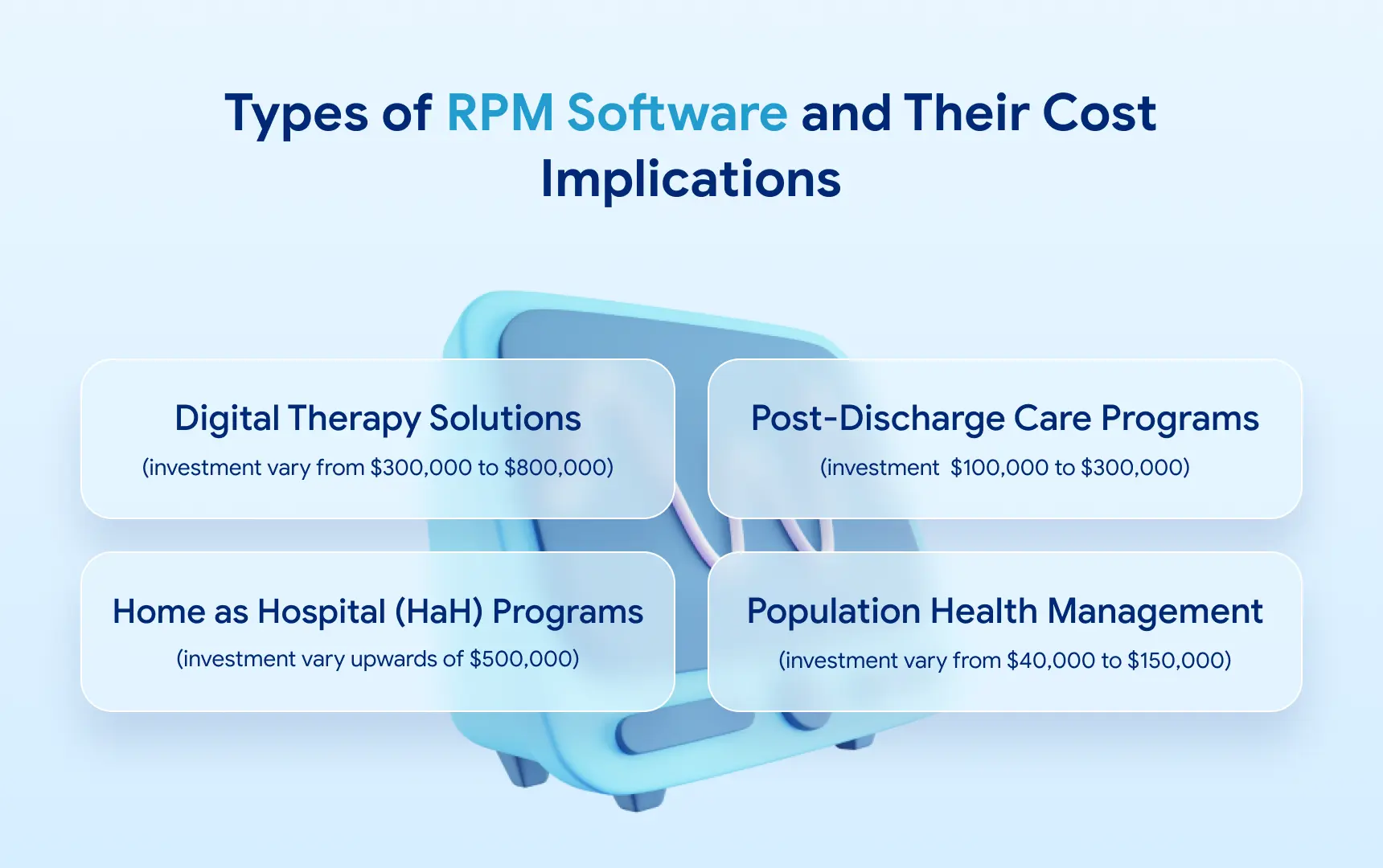
Digital Therapy Solutions
These telehealth apps and platforms are a direct line between doctors and patients. While their general focus is on consultations, such apps incorporate monitoring to ensure a patient’s stability post-therapy. It may involve tracking medication intake, monitoring changes in their vitals, and recording their feedback. The investments in such a solution may vary from $300,000 to $800,000.
Post-Discharge Care Programs
PDC solutions usually cover certain illnesses where treatment doesn’t truly end, even after surgeries or hospital stays. It overlaps with software that assists patients with chronic conditions, where constant, always-online monitoring is necessary. Such apps need precise collection algorithms tailored to the patient’s condition and status, which tends to increase costs. The cost of building a PDC solution is around $100,000 to $300,000.
Home as Hospital (HaH) Programs
This software relies heavily on a hospital’s systems, both those responsible for processing and uptime and those that collect data. However, it integrates with equipment placed in a patient’s home, which gathers the data and acts as the source. Such apps typically work as a complete replacement for hospital stays, so they are more complex and expensive. If you take into account both the software development and the sensors and wearables, you might have to pay upwards of $500,000.
Population Health Management
Especially relevant in the wake of a global pandemic, PHM software collects general vitals and health data from a broad array of patients and serves as an RSS feed for doctors. With these, medical professionals quickly gauge the status of many patients at once. Thus, they detect potential virus spread or track a whole city’s recovery from (for example, flu season).
The approximate cost of developing a PHM platform is somewhere between $40,000 to $150,000.
Exploring the Remote Patient Monitoring Cost in Details
Now that we’ve discussed the most widespread RPM types, let’s address RPM cost and what goes into it. We will break it down into two specific branches and cover each separately with a deeper explanation.
Initial Setup Costs and Equipment
This category seems the most intimidating at first glance, as it accounts for the big upfront spending you’ll face when starting with RPM. It involves creating an RPM solution, buying all the devices that will pair with that software, and getting the whole network up and running.
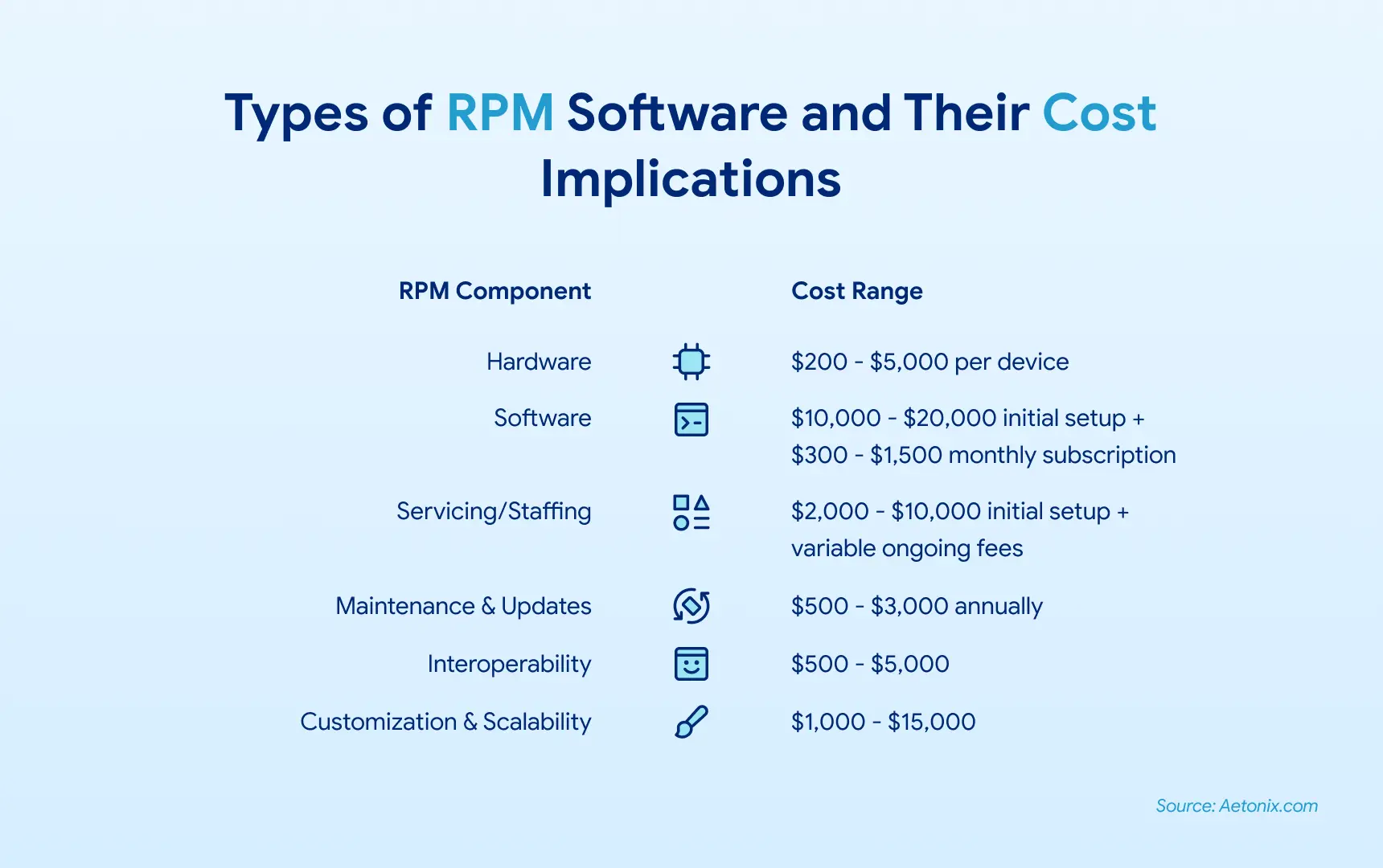
It’s vital not to go cheap on the equipment—buying knock-off versions or lacking a proper setup is too big a risk for your entire system. Granted, hardware can be pricey, costing between $200 and $5,000 per device. We’ll cover the more reasonable ways to minimize expenses in the cost of remote patient monitoring later on.
You’ll inevitably spend on sensors, server equipment, app development, and the integration of all the necessary third-party APIs. The software will likely cost you upwards of $10,000, while interoperability will range between $500 and $5,000. The latter depends on your required metrics and integrations. However, these costs are primarily one-time expenses. You will recoup them by running your RPM system.
After you finish the setup and buy all the necessary devices and software, you will still have to tune it. Experiment with various metrics and set appropriate benchmarks. This process takes time and money but ensures your solution works as intended.
Ongoing Operational Costs
Staffing and Support
Similarly, you’ll need to hire and maintain the staff that will operate the system on your side, which is another cost to accommodate. Ideally, keep the number of people to a minimum, banking on the quality of their training rather than quantity. A few specialists will keep the system up and running.
If you’d like an idea of how much the initial setup plus the actual staffing total, a study in Australia assessed the cost at $505 per patient. Note, however, that this included just one manager that handled the software.
Also, remember some other costs associated with getting end-users into the system and providing support. Helping people with the initial stages of using the system and learning how to use the associated app will be the most notable time sink and expense in the category. This can result in $2,000 to $10,000 initial spending, as well as monthly expenses. However, it’s possible to streamline the process.
Maintenance
Maintenance is yet another part of remote patient monitoring pricing to consider. No matter how efficient your system is, it will eventually need updates or fixes to stabilize and modernize it. That shouldn’t be a significant expense in the grand scheme of things, somewhere around $500 to $3,000 per year. You will likely offset it with the savings the RPM system provides.
Before we move on to the cost-cutting tips, here’s a breakdown of some base costs you’ll face:
In general, we understand that this list—equipment, training, ongoing maintenance—might seem daunting. However, there are ways to keep these expenses manageable, and we’ll discuss them next.
Get clarity on what you’ll need - and what you don’t.
Must-Have Integrations for RPM Success
For RPM software to function efficiently and support clinicians at scale, it must integrate with:
- EHR Systems (e.g., Epic, Cerner, or custom): to centralize patient records
- FHIR APIs & HL7 standards: for data exchange and device interoperability
- IoT Device SDKs: to connect with pulse oximeters, BP monitors, or smart inhalers
- Cloud Storage Providers: for secure, HIPAA-compliant data storage (AWS, Azure, GCP)
- AI Modules: to support predictive analytics or anomaly detection
These integrations enable real-time decision-making and reduce administrative burden. JetBase has implemented RPM integrations using both native SDKs and universal middleware across multiple platforms.
Strategies to Minimize RPM Costs
Nobody wants to pay more than necessary, mainly when the expenses can stretch over the years. Thankfully, these handy tips will help you save on the cost of remote patient monitoring. Take a look and see which of these apply to you.
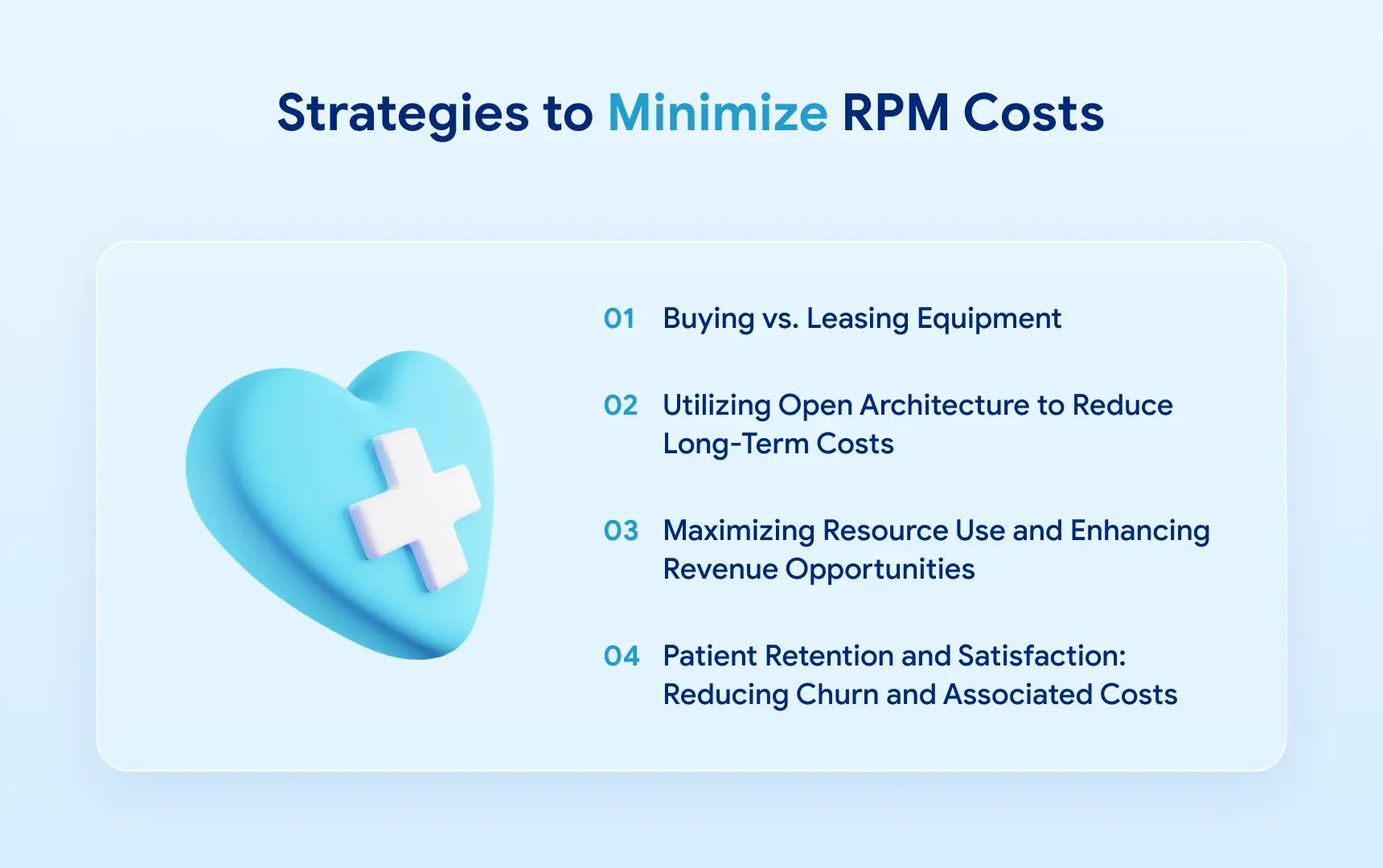
Buying vs. Leasing Equipment: Which Is More Cost-Effective?
The equipment that RPM systems require is quite specialized, meaning it’s hard to get used versions, at least in satisfactory conditions. That leaves most companies with two options: buying brand-new and rather expensive devices or leasing them long-term. It includes:
- Glucose meter
- Pulse oximeter
- Scale
- Blood Pressure Monitor
- Patient wearables
- Sleep monitors
- Thermometer
- Remote stethoscope
In our own experience, equipment integration to software costs around $1000-$5000, an intimidating price tag.
Utilizing Open Architecture to Reduce Long-Term Costs
Relying on open tech makes it easier to incorporate new types of devices and protocols. In contrast, proprietary tech and third-party software create the risk of vendor lock-in. Simply put, if you opt for open architecture, you’ll have more freedom to change your RPM solution and mold it to your needs.
Doing so is easier with a skilled team, which usually means outsourcing. But that’s just another way of cutting the cost of remote patient monitoring. Hiring a company from a different region to handle development, training, and maintenance while relying on open resources will inevitably be a money-saver. You could potentially cut your expenses by up to 30% this way.
Maximizing Resource Use and Enhancing Revenue Opportunities
Ensure all the resources associated with your RPM program are used efficiently. That is true not only for sensors and other equipment but also for people. Everyone’s skills should be employed to the max, with each doctor or intern able to work with the program and address minor issues when necessary.
This way, you save on keeping support staff available 24/7 and reduce the number of people required for the job. Such measures can ultimately save up to 20% of your budget.
It’s also worth thinking about reclaiming the cost with an effective revenue strategy. In addition to direct payments from patients or insurers, consider using the data you glean from the RPM system to improve your services further. Lower expenses will lead to more cost-cutting and optimization.
Patient Retention and Satisfaction: Reducing Churn and Associated Costs
RPM's nature and costs mean that any patient dropping out of the program is an extra expense. After all, you spend time configuring the software, setting up the sensors, and getting the wearable gadgets, which adds up quickly. The cost per patient goes up to $1000. Therefore, it’s crucial to keep patients invested in this system and fully see the process through.
Ensure each patient knows what they’re getting into and pay special attention to RPM's “onboarding” phase. Each participant should feel comfortable and understand the system's benefits personally. Then, you can lower the turnover rate and, thus, slash expenses. This is proven with long-term studies, where patients’ involvement in the program results in lower cost per patient, up to $20,000+ per year.
Understanding RPM Reimbursement and Return on Investment
The implementation of RPM solutions goes beyond monetary value because it delivers substantial worth.
Healthcare entities in the United States achieve Medicare coverage for RPM services through the use of CPT codes 99453, 99454, 99457, 99458. An RPM solution generates $100-$200 or more revenue per patient each month as recurring income.
The EU and UAE provide value-based care and digital health incentives that focus on chronic disease management and post-operation monitoring.
A well-designed RPM platform leads to annual savings of $20,000+ for each patient when it improves medical results and lowers emergency department use and allows early intervention (source: CDC, Philips, McKinsey).
Quote: JetBase recommends using readmission reduction rates, as well as adherence and patient satisfaction metrics, to demonstrate the effectiveness of digital health investments.
Need Remote Patient Monitoring Software?
Throughout this guide, we’ve shown our general knowledge of RPM and the healthcare industry, but you may wonder where that comes from. Well, JetBase has been creating software for over a decade, and many of our projects are in the medical industry. For example, we’ve made a telemedicine app, part of the RPM niche, with sleek UI and multi-tenant support.
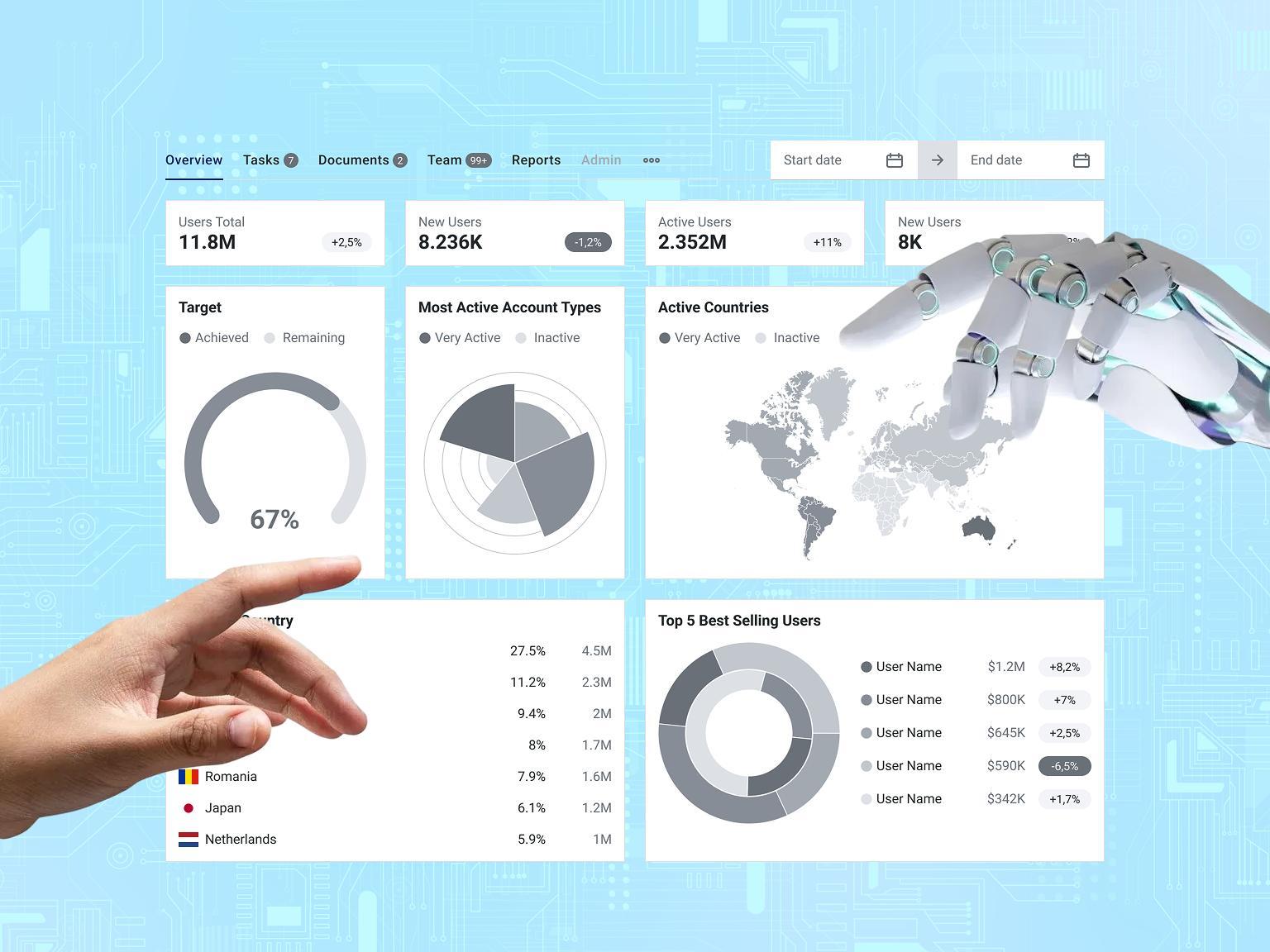
In addition to that tele-therapy solution, we have more RPM works, such as this one. It’s a SaaS platform that assists doctors with keeping tabs on patients in real time, with updates coming every second. Despite the constant flow of information, the app is lightning-fast as we optimized it for scalability. Using Flutter, our developers have made the cross-platform solution simple, lightweight, and convenient for patients and doctors.

Guaranteeing the app connects smoothly to various sensors that gather data such as lung capacity and blood glucose was an exciting challenge. Our engineers included detailed instructions that help patients handle the process and troubleshoot minor issues. As a result, the RPM program was cost-effective and had a limited need for support staff.
Conclusion: Is RPM a Worthwhile Investment?
While remote patient monitoring pricing can be somewhat steep, we’ve shown you ways to reduce costs. Follow our tips to launch your monitoring program without stretching your budget. If, however, you’d like some practical help in addition to our guide, you know whom to turn to.
We already discussed our projects, so we won’t make it long. You know our skills and your needs, so let’s match our capabilities to your project. Whether you need new RPM software or maintenance on your current one, we can handle it. Get in touch now to start our collaboration.