Any institution or business needs money to keep running and provide its services. Public health is no exception. Revenue cycle optimization helps ensure that the business processes patients efficiently and gets through the billing processes equally fast. It’s important to strike a balance between running a well-oiled payment mechanism and providing enough care to the patients. Today, we’ll teach you how to do just that.
JetBase’s guide to revenue cycle optimization will teach you how to overcome the common challenges in revenue cycle management (RCM). We’ll tackle the best practices that tighten revenue cycles, as well as pick apart the core components of RCM. As is often the case, relying on modern technology is the best way to get stellar results.
What Is Revenue Cycle Optimization in Healthcare?
Simply put, revenue cycle management optimization is a collection of actions that a business takes to improve the efficacy of patient processing and billing. It’s not about rushing the patient through the hospital system but rather about making the bureaucratic side of things less pressing.
Things like insurance verification, claims submission, and tons and tons of paperwork are hassles, both for the hospital and the patient. Streamlining these processes and letting doctors focus on treatment and easing patients’ minds is a double-sided benefit. Revenue cycle optimization here isn’t just automating steps but giving staff the tools to make their own efforts more efficient.
The Importance of Revenue Cycle Optimization
While reports show a general rise of up to 15% in hospital revenue and better margins, it’s crucial to understand that this is the result of hard work. Institutions that manage to leverage revenue cycle optimization in healthcare and minimize expenses tend to win big. However, those who let expenses get out of control report losses of up to several billion a year.

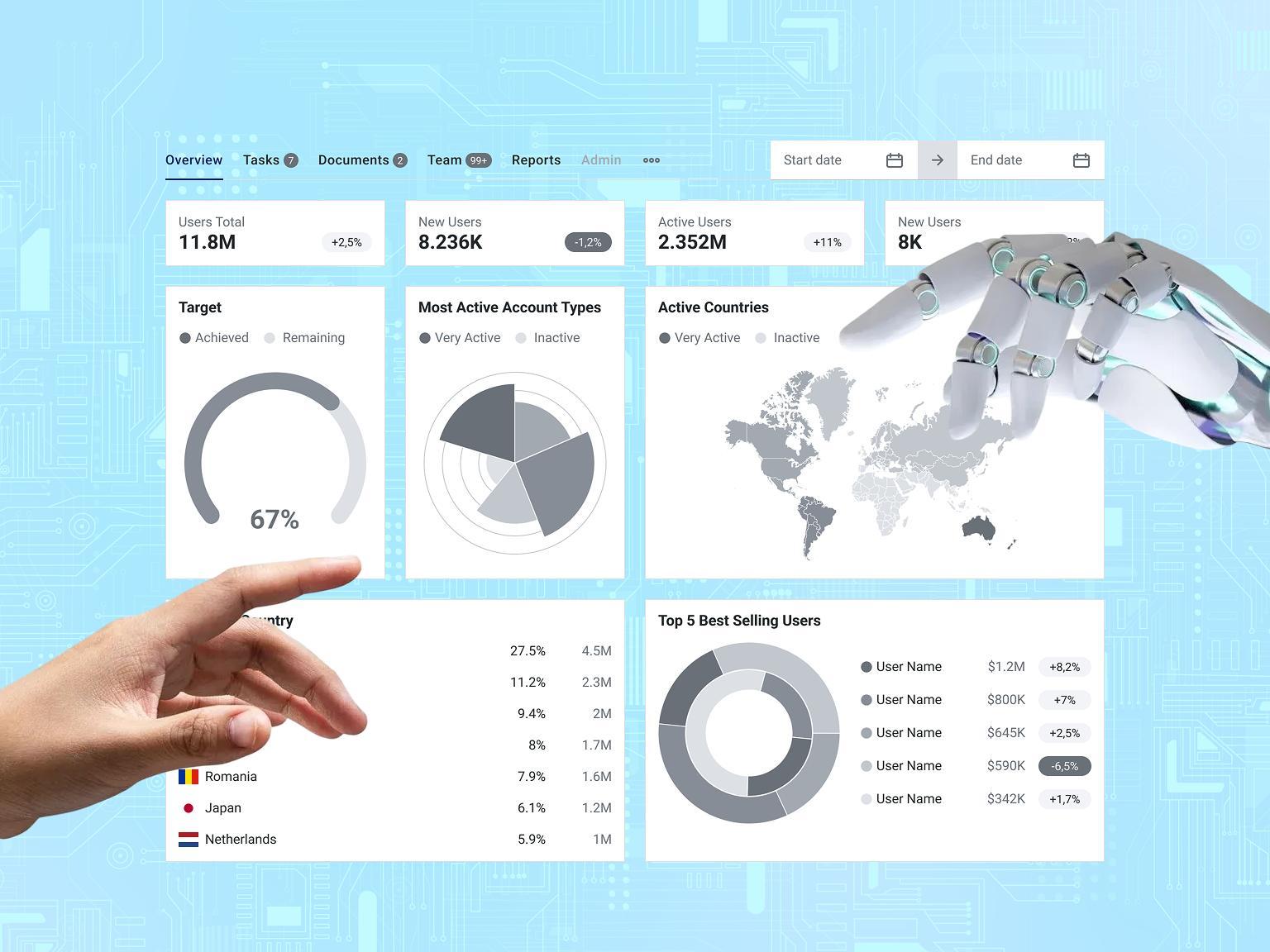
It’s hard to overstate the value of cutting off excess steps and raising margins, especially when the numbers speak for themselves. Using artificial intelligence (AI) or continuous staff training, a medical business should be able to reinvent its operations and angle them toward higher income.
How Automation and AI Enhance Revenue Cycle Optimization
Automation and AI technologies are revolutionizing revenue cycle optimization in healthcare by streamlining administrative processes, reducing human error, and accelerating the overall revenue cycle. With the advent of machine learning and robotic process automation (RPA), tasks such as patient billing, claims management, and payment processing can be automated, freeing up valuable human resources for more strategic roles.
For example, AI-driven analytics can predict denials and automate re-submissions, increasing the likelihood of successful claims. Additionally, AI can analyze vast datasets to uncover inefficiencies in the revenue cycle optimization, offering actionable insights that improve cash flow and reduce accounts receivable (AR) days.
Use Cases of Revenue Cycle Optimization:
- Claims Denial Management: A hospital that uses AI to analyze historical claims data can predict which claims are most likely to be denied. By automating the re-submission process with corrective measures, the hospital reduces the denial rate by 20% and improves revenue recovery.
- Patient Billing Automation: A large healthcare provider integrates RPA into its billing system to automatically generate and send out bills. By automating this process, the organization reduces manual billing errors by 30% and cuts down the time it takes for patients to receive their bills by 50%.
- AI-Driven Predictive Analytics: A mid-sized clinic adopts AI to predict patient payment behaviors based on historical data. The clinic uses this insight to offer personalized payment plans, increasing the patient collection rate by 25% and reducing outstanding balances.
- Automated Eligibility Verification: A healthcare organization uses RPA to automate insurance eligibility checks. This saves time for administrative staff and ensures that claims are submitted with accurate coverage details, reducing rejected claims by 15%.
Useful Points:
- Claims Processing Automation: AI-powered tools can auto-flag claims for quick resolution, significantly reducing the turnaround time for reimbursements.
- Predictive Analytics: AI can identify patterns in denials and patient payment behaviors, allowing healthcare providers to adjust processes proactively.
- Error Reduction: Automation minimizes manual data entry, reducing human errors that can result in costly claim rejections.
- Patient Payment Automation: AI tools can send automated payment reminders to patients and offer personalized payment plans, improving collection rates.
COVID-19's Influence on Revenue Cycle Optimization
The COVID-19 pandemic has had a profound impact on revenue cycle optimization in healthcare, forcing many organizations to reassess their financial processes and implement more agile, technology-driven solutions. With increased telehealth adoption, new coding requirements, and fluctuating patient volumes, revenue cycles became more complex.
As healthcare providers grappled with these changes, automation and AI emerged as critical tools to streamline billing, claims processing, and patient engagement. This accelerated the shift toward digital transformation, where remote billing teams, AI-driven denial management, and telemedicine reimbursements became standard practices.
| Influence Area | Impact of COVID-19 |
|---|---|
| Telehealth Billing | New coding regulations and reimbursement models introduced. |
| Payment Delays | Increased patient financial responsibility due to unemployment. |
| Claims Processing Efficiency | Higher demand for automation to process surging claim volumes. |
| Staffing Changes | Shift to remote billing and coding teams for cost efficiency. |
| Denial Management | Increased denials from new, complex regulations and coding errors. |
Valuable Insights:
- COVID-19 accelerated the need for AI in telehealth billing, ensuring compliance with rapidly changing regulations.
- Automation tools have become crucial for managing remote teams and streamlining tasks like claim re-submissions and patient engagement.
- The pandemic pushed healthcare organizations toward more proactive financial planning, relying heavily on real-time data analytics to forecast revenue trends and payment risks.
Key Components of Revenue Cycle Management
To improve revenue cycle management, you’ll need to account for its key components. Before we discuss the process's hurdles and methods, let’s discuss those components and why they’re important.
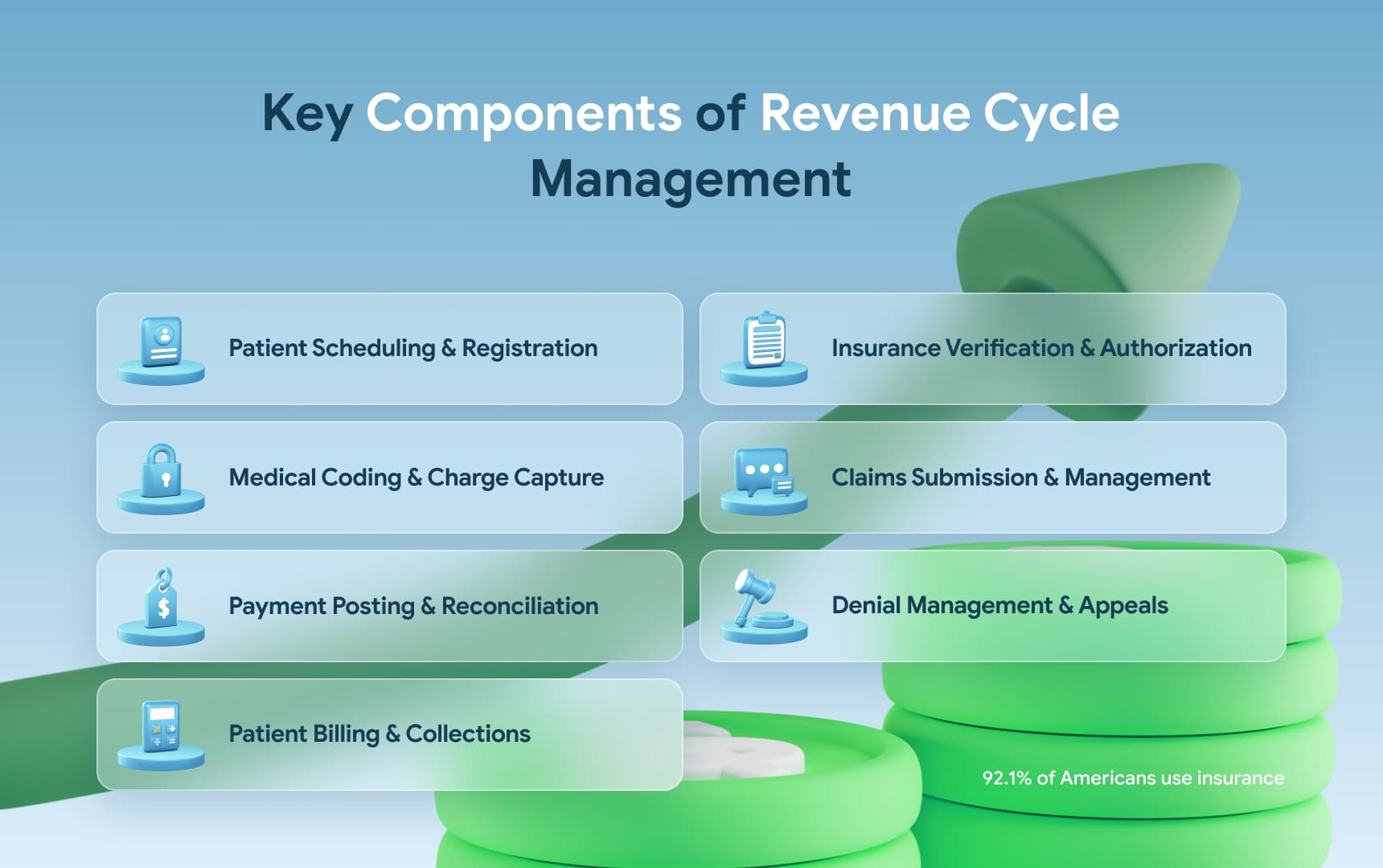
Patient Scheduling and Registration
From the moment a patient decides to use your services, revenue cycle optimization begins to take effect. Too many institutions make the act of scheduling a doctor’s appointment or filling out the paperwork tedious. This wastes precious time and, thus, money. It’s important to use simple templates and online systems for this in order to cut the expected time-to-visit.
Insurance Verification and Authorization
Insurance is a vital part of medical procedures nowadays, with 92.1 percent of Americans using it at some point during the year. Thus, it’s important to create integrations that automatically process a patient’s insurance. These should verify that the policy is active and the patient is authorized to use it.
Such integrations must be scalable and support verification for many patients at a time. This is easiest to achieve with a cloud infrastructure. It will also allow you to store all relevant data in a way that makes it accessible to all branches of your institution. Using such multi-purpose solutions is the essence of revenue cycle management optimization.
Medical Coding and Charge Capture
Medical coding is about assigning shorthand codes to standard medical procedures, making it easier to record and track them. Which, in turn, leads to the charge capture part of the revenue cycle optimization. This involves reading the code data to calculate services rendered and compile a bill.
Creating a system that automatically pulls info from a database based on the shorthand will speed up the whole process. Similarly, if certain services are often provided in a group, creating presets that calculate such groupings makes sense. For example, a patient who gets blood drawn will likely have specific blood work done, resulting in a grouped code.
Claims Submission and Management
In an ideal world, submitting a claim to your patients’ insurance companies would be a breeze. You can create solutions that automatically fill out a patient’s info and list services that you’ve provided. However, an error at this step could lead to a claim getting mired down in bureaucracy and rejected multiple times before it finally goes through.
This is why it’s important to combine both automated, technology-reliant solutions and staff training if you want to improve revenue cycle management. Prioritizing a melding of employee skills with your software and streamlining the routine parts of the work is the ideal approach.
Payment Posting and Reconciliation
This step of the cycle is about receiving compensation, tallying it up, and comparing it to amounts owed. At that point, it’s vital to not just spot a discrepancy but understand how it happened and how it can be fixed most efficiently. Here is how to improve revenue cycle management at this stage: consider AI analysis.
Such tools can help quickly sort through incoming payments and information. They’ll not only spot the difference in numbers expected versus numbers received. These can also understand statements from the insurers and summarize them to highlight problems quickly.
Thus, you speed up resolutions and avoid the long wait for full reimbursement.
Denial Management and Appeals
On occasion, during the cycle, a hospital receives claim denials. It’s obviously not an option to simply leave bills unpaid, and this calls for an appeal. For this step, healthcare revenue cycle optimization begins with understanding the common denial reasons. This can be done with some long-term data analysis.
Then, when you clearly know which claim denials are most common, your solutions can automate parts of the appeal process. This way, each denial doesn’t cost as much time, and the disruption to your regular cycle is minimal.
Patient Billing and Collections in Revenue Cycle Optimization
When all the claims and insurance payouts are processed, it’s possible that a patient will still have some outstanding debts to the hospital. This last step of the cycle involves tallying them up and collecting them. In the sense of revenue cycle optimization it’s one of the more challenging areas as the human factor makes it unpredictable.
However, it can be simplified with template bill claims and auto-collection notices.
Common Challenges in Revenue Cycle Management
As with any complex process, RCM has its own unique risks and issues. Tackling them is an essential part of revenue cycle optimization, so let’s get to know the core ones. While you might face some unique ones, these five are the standard problems that most medical institutions run into.
Inefficient Processes
This can range from completely disorganized workflows to processes that could be tightened by just 5 to 10% to reach perfection. Regardless of scale, healthcare revenue cycle optimization dictates you need to find ways to streamline each process. From calculating payouts to sending out claims, it’s crucial to cut excess time and effort.
Inadequate Staff Training
The human factor can influence your bottom line greatly, as unskilled employees won’t make the most of the advanced tools and techniques you give them. This is why revenue optimization in healthcare requires continuous improvements in your staff. From on-site training to comprehensive guides, it’s important to offer varied learning options.
This way, you speed up the revenue cycle, prevent errors, and even enhance security. An employee familiar with the system won’t accidentally leave data exposed. Moreover, they can create their own optimal workflow to finish payout tasks extra quickly.
Compliance and Regulatory Issues
Processing payments will inevitably involve sensitive patient data, which falls under HIPAA, GDPR, and the like. As a result, your revenue cycle optimization must account for the fact that certain compromises must be made.
This involves data storage, meaning you might not be able to hold on to payment information. Therefore, your staff must re-enter data if a patient returns for more procedures, creating extra work.
Technology Limitations
A lot of hospitals run on legacy systems and hardware, making genuine revenue cycle optimization difficult. After all, there’s only so much you can do without modernizing it all. Rehauling the system may be costly initially, but it creates a lot of value and opportunity in the long run. Plus, you can save by outsourcing the work to a skilled team.
Patient Payment Difficulties
Sometimes, patients are reluctant to pay or simply lack the funds. Navigating these complications is a necessity, and you can take steps to mitigate the slowdown. For one, it’s possible to offer installment payments with automated software handling the process.
Hospitals can also set up alerts to remind patients about overdue bills. It’s not the most glitzy part of revenue cycle optimization, but a crucial one nonetheless.
Best Practices for Revenue Cycle Optimization
Now that we described some of the common challenges let’s consider how to cope with them. Those who want to know how to improve revenue cycle can simply follow these methods to reorient their systems. Technology-based solutions will limit the payment processing time and speed up the cycle's bureaucratic parts. Read on to find out how.

Workflow Improvement
While it’s common for staff members to have their own unique approaches to work, it’s still important to set general guidelines. These should include tips on cutting out extra steps and distributing tasks so that everyone’s workload is even. Revenue optimization in healthcare assumes that everybody is operating in tandem, like a well-oiled mechanism.
Digital Transformation
Forget about paper and analog systems if you want to truly optimize. Take your systems online or, better yet, take advantage of cloud computing. It will not only guarantee that your information is safely backed up but also enable you to use modern, high-speed solutions.
Healthcare revenue cycle optimization cannot happen without fresh technology cutting off outdated processes.
Staff Training and Development
It’s important for your employees to keep pace with any changes you make to the internal systems. You can start by teaching employees how to navigate systems on a daily basis. But remember to also train them to deal with errors and challenges. It’s important to also listen to employee feedback as they get the hang of your digital solutions.
They’re vital players in your revenue cycle optimization, and you must accommodate their needs and ideas.
Medical Coding Improvement
We’re not suggesting you abandon your coding system in pursuit of revenue optimization in healthcare, far from it. Instead, integrate them with your payment system. It should be possible to automatically calculate a patient’s bill within seconds of the listed procedures.
Managing specific combinations of codes that tend to pair with one another is also a way to speed up code processing.
Implementing Artificial Intelligence (AI) Solutions
Another point on the technology adoption for revenue cycle optimization is the use of AI to process data more efficiently and automate steps of the cycle. This can include simple communication with patients, such as payment reminders or insurance claim posting.
Similarly, trained AI can comfortably handle basic patient registration or code logging, following templates that you set.
Leveraging Data Analytics
High-scale analytics can help you understand the payment cycle better and find ways to tighten it. From analyzing insurance payout rates to spotting the most time-consuming aspects of payment processing, analytics give you hard data and ground to build on. It also helps prevent revenue leakage, where potential revenue is lost due to missed payments or inefficient processing.
Payment Posting and Reconciliation Automation
Speaking of which, it’s no surprise that automating repetitive tasks is the easiest way to do revenue cycle optimization. You don’t need to have staff routinely sending out invoices and notices when software can handle this process just fine.
Custom development for healthcare is readily available and will save uncountable hours as well as money.
Claims Management System Implementation
With thousands of patients a day, large hospitals should seek ways to streamline their communication with insurance companies. This is where claims management software comes in, offering ways to speed up claim submission and processing.
The system should let you easily see the status of many claims at once, filter them, and do bulk actions.
Measuring the Success of Revenue Cycle Optimization
After you implement these practices for healthcare revenue cycle optimization, it’s important to assess their effect on your institution. You obviously want to see major improvements as a result of these changes. Here’s how to track them and handle the post-optimization period.
Key Performance Indicators (KPIs) to Track
There is a standard set of KPIs that will help you assess how well your system runs. We won’t list all of them but only the most important ones, such as:
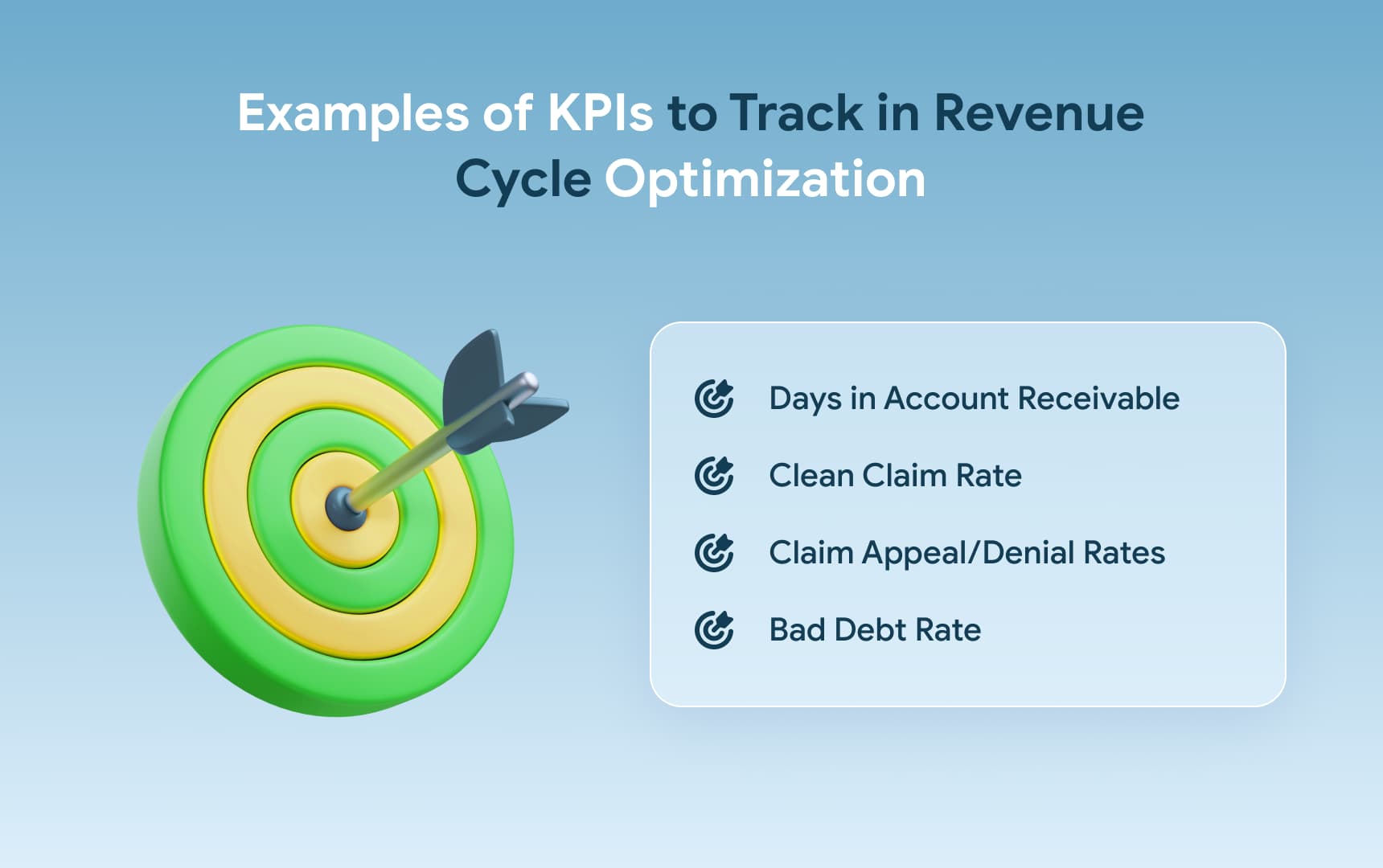
- The first one reflects how long it takes for you to receive a payment on average. This means a lower metric is ideal, as it signifies quick, efficient cash flow with no time spent on appeals.
- The second stat is similar, as clean claims are ones that are simply paid on request. They aren’t bogged down with appeals or denials. If their number goes up, you did revenue cycle optimization right.
In contrast, the appeal/denial rates should be kept as low as possible for obvious reasons. If you’re using an automated system, you will likely see them decrease.
However, it might also make sense to tweak the algorithms to see if further changes will bring it down even lower.
Lastly, bad debts are ones left unpaid permanently and you do not want to see them go up, ever. Once you run some healthcare revenue cycle optimization practices, bad debts should decline permanently.
Regular Performance Assessments
While KPIs show how well your system runs and how much it benefits you, we’ve said earlier that employees are just as essential to revenue cycle optimization. It’s crucial to include performance checks and make sure that staff is keeping up with the changed system.
No matter how much automation you do, they have to provide high-quality work in order to boost KPIs.
Continuous Improvement Plans
Don’t stop after just one round of improvements, as regularly scheduled software updates can keep metrics going the right way. This is both about implementing new features and simply reconfiguring your software once in a while to test new things. Your revenue cycle optimization may give great results right away, but experimenting is a great opportunity to improve them.
If you want your revenue cycle optimization to be successful, you can turn to a team with experience. JetBase has spent over a decade crafting custom solutions and helping companies with digital transformations. We can implement AI features for your revenue cycle, enhance it with data analytics, and take your enterprise to the cloud. Contact us now to start work on your project.
Healthcare Revenue Cycle Optimization Costs
Optimizing the healthcare revenue cycle comes with both short-term investments and long-term cost-saving benefits. Implementing automation tools, AI-driven analytics, and comprehensive training programs for billing teams requires an upfront financial outlay, but the returns in efficiency and reduced operational costs often justify the expense.

Typical costs involve software procurement, customization for specific workflows, and ongoing system maintenance. However, optimized revenue cycles reduce AR days, improve claim approval rates, and enhance patient payment collections, resulting in significant financial improvements for healthcare organizations.
| Cost Element | Estimated Investment |
|---|---|
| Automation Software | $50,000 - $200,000 (depending on provider size and scope) |
| AI Analytics Tools | $25,000 - $100,000 for advanced predictive analytics tools |
| Employee Training | $10,000 - $50,000 for training on new systems and processes |
| Maintenance and Support | 10-20% of software costs annually for system upkeep |
| ROI from Optimization | 20-40% reduction in AR days, improved collection rates |
Valuable Insights of Revenue Cycle Optimization Costs:
- The initial cost of automation can be steep, but healthcare organizations typically see a return on investment (ROI) within the first year through faster reimbursements and reduced errors.
- AI-driven insights offer long-term cost benefits by improving denial management and allowing for more accurate forecasting, reducing financial risk.
- A well-implemented revenue cycle optimization program can reduce operational costs by automating repetitive tasks and lowering staffing needs for billing and claims processing.